Volume 5, Issue 1 (3-2021)
EBHPME 2021, 5(1): 29-42 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Nasiri T, Hosseini-Shokouh S. Productivity Trend in Iranian Health Sector: A Descriptive Approach. EBHPME 2021; 5 (1) :29-42
URL: http://jebhpme.ssu.ac.ir/article-1-306-en.html
URL: http://jebhpme.ssu.ac.ir/article-1-306-en.html
1. Health Management Research Center, Baqiyatallah University of Medical Sciences, Tehran, Iran 2.Faculty of Health, Baqiyatallah University of Medical Sciences, Tehran, Iran , hosainysh.morteza@gmail.com
Full-Text [PDF 719 kb]
(612 Downloads)
| Abstract (HTML) (1640 Views)
Full-Text: (346 Views)
Background: Low productivity and consequently increased health costs can cause various problems in society and the welfare of individuals. The first effect of the high cost of production in the health sector is the collapse of hospitals and health centers into a cost-inflation spiral.
Methods: This was a descriptive-analytical study. A review section has been revised to describe the concept of productivity through narrative literature review in the descriptive section, using the time series data of 1991-2012 of the Statistics Center of the Islamic Republic of Iran. The micro and macro indicators of health economy and health sector productivity are presented and analyzed graphically with the help of Excel software
Results: From the economic point of view, productivity is defined as the ratio of output to input. The results showed that inflation in the health sector was higher than general inflation in the period under study and that out of pocket expenses were made to cope with inflation in the health sector. On the other hand, the growth rate of production in the entire health sector was decreased, and the number of physicians and bed potency was reduced.
Conclusion: The final result of this study showed that the productivity of the health sector is not in good condition. Despite the increase in the number of beds and doctors in the last two decades, the added-value and production of the entire health sector have not grown significantly.
Key words: Productivity, Trend analysis, Health sector, Iran

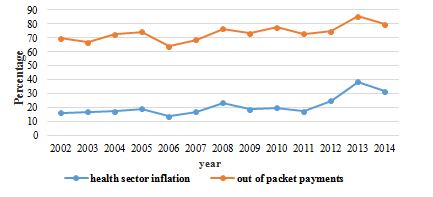
Figure 3. Concurrent Inflation of Health Sector and People's Out of Pocket Payments (Source: Study Findings)

Figure 4. Added-value and Total Health Sector Production Trend (Source: Study Findings)
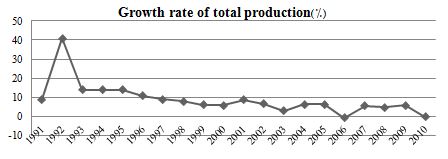
Figure 5. The Growth Rate of Total Health Sector Production (Source: Study Findings)
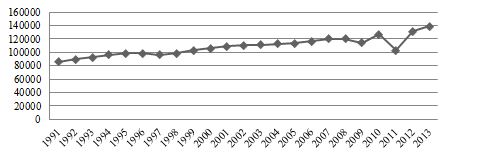
Figure 6. Bed Count Trend (Source: Study Findings)

Figure 7. The Growth rate of beds (Source: Study Findings)
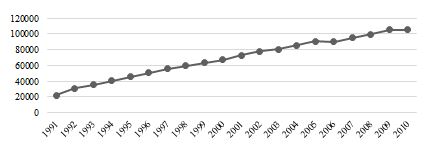
Figure 8. Trend Number of Physicians (Source: Study Findings)

Figure 9. Bed Productivity Growth Rate (Source: Study Findings)
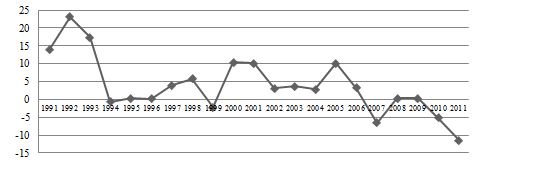
Figure 10. Physician Productivity Growth Rate (Source: Study Findings)
Discussion
As most scientific literature has shown, the most feasible way to measure a system's productivity is to calculate the input-output ratio. The current study used this relationship to derive physician and bed productivity in the health sector. The final result of this study revealed that the productivity of the health sector was not adequate. Despite the increase in the number of beds and physicians in the last two decades, the value-added and the total production of the health sector have not grown significantly. Through these terms, the authors refer to the production of the whole health sector, the real value of the total services, and marginal products produced in the health sector (33, 34).
However, this study did not judge health system performance because according to the World Health Organization report in 2000, three general indicators for measuring health system performance are outlined, i.e., the level of public health, the accountability of the health system, and protection against financial risks. The health system's performance models refer to efficiency (productivity) as an intermediate target (35, 36). Therefore, in the current research, only the efficiency and productivity of the health sector of the country are examined. Poor productivity of the country's health system can be due to various reasons. These reasons can be classified into two categories: micro and macro. In the micro sector, i.e., hospitals and healthcare centers' level, the first cause of low productivity can be attributed to the lack of full utilization of inputs. In health centers, various types of inputs such as labor, beds, medical equipment, buildings, energy, and so on are used in the service production process. If health centers are not at the frontier of utilizing these inputs, they will be inefficient in the production process and cause loss of resources. Energy is one of the factors that inefficiently utilize the production process in the health sector, especially in public health centers. In some public health centers, due to the depreciation of buildings, energy consumption is extremely high, leading to inefficiency (12, 23, 37-39).
Another reason for the low productivity in the health sector can be found in market theory. The public sector is far from market-driven. One of the characteristics of markets is that they allocate resources efficiently and exploit each resource based on its final output. This allows the density of the use of inputs in firms to be distributed efficiently and is based on maximum productivity. In government health care centers, the way that resources are combined to produce services are not market-based and is far from technical and economic measures of production. This causes the inputs not to be used according to their production capacity. Therefore, based on the findings, it can be concluded that despite the increasing number of inputs over time the output of the health sector has decreased (23, 39).
One study claims that applying different policies, even in similarly structured systems such as Italy and England, will make a difference in the efficiency of the health system. The NHS growth rate for the whole period (2004 to 2011) increased by 10 % and an average of 1.39 % per year, while overall SSN productivity increased by 5 % at an average of 0.73 % per year. Our results show that different policy goals have different outcomes for the two countries. In the UK, the NHS has focused on increasing activity, reducing waiting times, and improving quality. Contrarily, Italy is more focused on cost containment and rational provision in the hope that it will render unfair and inadequate services. The findings of this study differ from our study findings in terms of the rate of change while examining different inputs and outputs (13). At the macro level, lack of evidence-based policymaking, cross-sectoral disagreements, lack of competitive incentives in the health sector, lack of complete and transparent buyer separation from the provider, weakness of the health sector financial system, etc. are noted as factors of reduced productivity. The lack of strategic purchasing in the health sector has made the cost of services not close to their true value, and providers are demanding unrealistic tariffs and basing prices on their monopoly power, especially in the public sector. In such an environment, no health care product will have the incentive to improve productivity and reduce cost (23, 39-41). Addressing all the factors of low productivity is beyond the scope of this article. Therefore, some undesirable effects of low productivity are discussed below.
Low production efficiency (lack of optimal use of health system labor, equipment, and resources, etc.) makes the cost of health services high and causes inflation in the health sector (40, 41). In addition to this, in Iran's health system, the wage gap and price productivity have been drained due to higher wages than staff productivity. In economics, this rule is referred to as the Baumol theory. According to this theory, the growth rate of prices in an industry is equal to the difference between the growth rate of labor productivity and the growth rate of wages. The inflation of the health sector and the higher inflation of this sector of the whole economy are evidence of this phenomenon. As shown in the previous section in Figure 1, the inflation of the health sector has been higher than general inflation in recent years. The findings of Ahmadi et al. study of the years 1995 to 2007 were similar to the present research showing that the inflation of the health sector has always been higher than the public sector in Iran, but has not been a consistent trend in public and private tariffs (12). Another study in the US found that issues such as general inflation, population growth, population changes, increased per capita public health, and intensive care services have been instrumental in raising consumer prices in the health sector (42). Some other studies have reported incomplete insurance coverage and the share of people paying premiums as factors in increasing health costs (43). Other researchers believe that increasing insurance coverage will cause technological changes and ultimately increase health costs (44). Newhouse categorizes these inflation factors into two groups of demand-side that include community aging, expansion of insurance coverage, and supply-side category that consist of inducing demand, growth in productivity, and insurance companies' management and technological change (45). Therefore, higher inflation in the health sector than in the public sector has been confirmed in most of these studies. In addition to the factors mentioned earlier, factors such as the increase in the quantity and quality of hospital hotels, more specialized human resources, etc. should also be added to Iran's list (12). A study in Norwegian hospitals shows that the rate of physicians' productivity declined between 2001 and 2013, followed by health reforms. The main reason for this is the lack of the support of nursing staff and ward secretaries (46). According to the OECD productivity survey, the main reasons for the increase in Denmark and Canada's productivity are the technical changes (9). In another study for OECD countries, the main causes of inefficiency in health care were factors outside the control of the health system, including GDP, education, smoking habit, and obesity. High inflation in the health sector coupled with the lower purchasing power of the population either pushes the burden of financing rising health care spending on the public budget or increases the catastrophic health expenditure spending and out-of-pocket payments resulting in poverty from health spending. The concurrent movement of inflation in the health sector and the amount of out-of-pocket of the population shows that the inflationary pressure of the health sector in Iran has been on the rise in recent years. Low productivity can also affect the quality of health services (12, 47).
Ancarani et al. (16), in reviewing the technical efficiency of Italian hospitals, found that managerial decisions to use more resources than external factors had a greater impact on health efficiency. Gunnarsson et al. (48) have evaluated the efficacy of these costs by referring to the magnitude and importance of government health and education costs in countries. They attribute the underlying causes of countries' inefficiencies to inadequate access to real resources such as teachers and medicine and also point out that higher costs will be associated with lower efficiency. Alin O, Marieta analyzed the economic efficiency of the health system in Europe using health indicators and the ratio of health costs to GDP and concluded that the average health expenditure efficiency in the European :union: was less than one, concluding that its benefits were lower than the costs (49). A comparison of the average efficiency of public and private health expenditure in the countries of the region and North Africa (MENA) claims that the efficiency of private health expenditure has improved over the 2005- 2010 period and the gap between the efficiency of these two types of expenditure in the health sector has declined. The main reason for this is the reduction of public expenditure efficiency on the one hand and the improvement of private expenditure efficiency on the other. The lowest and highest average technical efficiency of public health expenditures were related to Jordan and Yemen, respectively. In contrast, the lowest and highest mean technical efficiency of private health expenditures is allocated to Lebanon, Mauritania, and Oman, respectively. This study continues to redefine public health expenditure, reform public health expenditure structure, revise the method of resource allocating health expenditure, and so on. On the other hand, it recommends helping improve the efficiency of private spending especially through the transfer of health units to this sector (7). Efficiency is one of the most important indicators of productivity. Measuring this index is a criterion for comparing the utilization of available resources against standard criteria or an index for assessing the performance of homogeneous and homogeneous units. The study by Rezapour et al. (50) showed that Southwest Asian countries suffer from economic inefficiencies due to the 12 % unproductivity of resources which is a result of poor efficiency of management, scale, and allocation. The study reported that the countries under investigation were able to access the same basic health indicators by using and allocating 88 % of the current health system resources. According to the World Health Organization, more than 50 % of resources in health care are inadequate (50). Robert's study (2008) of the inefficiencies of the OECD countries showed that the main reason for the weakness of productivity in health systems is the weakness in the allocation of health system resources (14). Evans (2001) attributed the inefficiency of health systems to the low cost of health care per capita. The results of some studies emphasize the role of management inefficiency (51). Good management is prominent in the health system, motivation, and effort of human resources for high-powered activity, training, and supply of human resources. The absence of a systematic assessment of the health system, lack of human resources in a position that is appropriate to their skills and education, lack of motivation for training promotion and specialization, lack of areas of creativity and variety, etc. can all affect the efficiency of human resources (8, 9). Another study does not consider the cause of low efficiency and increased costs in specialist workforce shortages but rather focuses on factors such as lack of utilization, maintenance and support, how resources are allocated at different levels, and how much they spend to improve health system performance. Overall, these studies emphasize the role and importance of managers in enhancing performance (9). Therefore, poor production makes the services provided in the health sector not of good quality and effectiveness. This may affect other health performance indicators (12).
Conclusion
In conclusion, suggestions for improving the productivity of the health sector are as follows:
The authors thank Dr. Ahadinezhad for providing the data and the preliminary idea of the manuscript.
Conflict of interests
The authors declared that there is no conflict of interests in the present study.
Authors' contributions
Hosseini-Shokouh SM designed research; Nasiri T conducted research; Nasiri T Analyzed data; Hosseini-Shokouh SM and Nasiri T wrote manuscript. All authors read and approved the final manuscript.
Funding
Non applicable
Methods: This was a descriptive-analytical study. A review section has been revised to describe the concept of productivity through narrative literature review in the descriptive section, using the time series data of 1991-2012 of the Statistics Center of the Islamic Republic of Iran. The micro and macro indicators of health economy and health sector productivity are presented and analyzed graphically with the help of Excel software
Results: From the economic point of view, productivity is defined as the ratio of output to input. The results showed that inflation in the health sector was higher than general inflation in the period under study and that out of pocket expenses were made to cope with inflation in the health sector. On the other hand, the growth rate of production in the entire health sector was decreased, and the number of physicians and bed potency was reduced.
Conclusion: The final result of this study showed that the productivity of the health sector is not in good condition. Despite the increase in the number of beds and doctors in the last two decades, the added-value and production of the entire health sector have not grown significantly.
Key words: Productivity, Trend analysis, Health sector, Iran
Introduction
In recent decades health systems around the world, without exceptions, have faced the challenge of inflationary pressures. The problem of rising expenditure of the health budget in our country has become more complex due to its dependence on oil revenues and consequently, the impact of oil revenue fluctuations on the health system performance. Fluctuations in oil revenues, in addition to affecting other parts of the country, have led to poor stability in health sector policies, particularly in the area offinance (1, 2).
Generally, several factors have been suggested increasing public sector expenses and pressure on the public budget (3, 4). Similarly, the health sector as an industry that converts inputs into products in the form of health services and goods must operate efficiently and be at the frontier of its production capabilities (5).
The issue of efficiency and productivity in the health sector is important both at the micro-level such as hospitals, and at the macro level, i.e., the whole health system. The importance of productivity in the economy and the country is well reflected in the policies of a resistive economy. The newest growth models are also the sole catalyst for sustainable economic growth in productivity growth. Based on classical microeconomic models, the point where the average production curve of a firm is maximized, the mean cost curve of the variable production is minimized, and at the point where the final cost of production is minimized, the final output is maximized (6).
Therefore, it is clear that efficiency and productivity play a key role in controlling costs, especially for firms such as hospitals. So far, no similar study has been conducted on the examination and analysis of health productiveness in the country, and most of the research work in this field has investigated and analyzed the efficiency of the health system at a micro-level (hospitals and healthcare centers). These include the studies of Azar, Hoseini Nassab, Sabagh Kermani, Karimi, Fattahi, Pirani, Kiani for efficiency and situational analysis of Rezapour's health system allocation and Ahmadi's inflation indicators in the health system (7-12). Moreover, related external studies include Atella and Färe, Roberts on productivity, Ancarani, Alin O, Marieta, Eling and Kirigia, Al-Shayea, and Chan on efficiency (9, 13-20). However, in some studies on health system productivity in developed countries, the average productivity growth is mentioned as about one percent annually.
They were quite different from the present study in terms of method and did not even provide a conceptual explanation of the subject. Hence, the present study is unique in this respect. Low productivity and, therefore, higher health costs can have various problems for society and the well-being of individuals. The first effect of the high cost of production in the health sector is hospitals and health centers' declination into a cost-inflation spiral (2).
Therefore, productivity and efficiency are some of the most fundamental areas in
the scientific environment of the country. Accordingly, in this article, the authors intend to illustrate the country's health system's efficiency and effectiveness. Due to restrictions on access to data on the inputs and outputs of the country's health system, this section presents a picture of the health system's efficiency for measuring the system's output from the added-value index and total output in addition to measuring inputs. The number of beds and the workforce has been used. Although other factors and inputs also play an important role in the output of the health sector, no relevant data were available in this study. For this purpose, this article is arranged into several sections. The first section provides an overview of the concepts of productivity. The second part discloses the efficiency and productivity of the country's health system. The final section discusses the reasons for the low productivity in the health sector, its impact on key performance indicators, and offers ways to improve productivity and reduce the costs of producing health services.
Materials and Methods
Study design and literature review
This was a descriptive-analytical study in which the concept of productivity was presented in the review section using specific keywords related to the concept of productivity and searching related internal and external texts in databases. Thus, the title and abstract of all Persian and English language articles from 2000 to 2019 were extracted and screened using valid search engines such as Science Direct, Scopus, Pubmed, Magiran, Irandoc, SID, Google, scholar, Medline, and Embase Cochrane databases. At first, a large search was conducted on the Google database with high sensitivity, and later the search was conducted using proprietary strategies of each database. Keywords related to the concept of productivity, such as productivity, effectiveness, efficiency, added-value index, total output, total production, bed inpatient, manpower, workforce, and labor were used to increase the adequacy of the samples. A list of articles and books was also searched using the same keywords. Other words such as "health system," "health policy," "health sector," "health care system," "inflation" were added to the search strategy to facilitate the search process. Qualitative studies were also reviewed in this screening. Initial screening of search results by title and abstract of studies was performed by one of the browsers, the second browser independently reviewed the studies found, and the consensus was reached in cases where there was disagreement. Overall, in the first stage, about 1050 studies were initially evaluated, from which 110 studies were purposefully selected and reviewed in the second stage. Texts that had more conceptual richness (referring to the definition and interpretation of productivity concepts and other related frontiers in the field, opposing, and similar concepts and their constructs), more recent sources, authoritative journals or databases, and valid references were the criteria considered to prioritize studies (21, 22). Resources explaining the concept of productivity in other areas were excluded from the studies. Accordingly, the studies were ranked and studied in order, and finally, 20 articles were eligible for inclusion in the study, which was in full relation to the subject under study.
Total production is the maximum amount of product that can be produced with any given combination of variable and fixed inputs. On the other hand, value-added in simple language is the difference between output and input. As most scientific literature has revealed, the most practical way to measure the productivity of a system is to calculate the ratio of output (total production and value-added) to input (bed and physician) annually. In the current study, this relationship was used to extract physicians and beds' productivity in the health sector. Finally, all data from articles were extracted and screened.
Data sources and analysis
In the descriptive section, information regarding the statistical center of the Islamic Republic of Iran, the microeconomic and macroeconomic indices of health and productivity of the health sector from 1991/2 to 2011/2 were presented graphically and analyzed with the help of Excel software. Data after 2012 was not available.
The authors declare that they have complied with the principles of the Helsinki Declaration.
Results
Productivity concept
Productivity is defined as the power of production and being productive (23). In the private and commercial sectors, productivity is measured by factors such as product quality, resource effectiveness, and customer satisfaction (24). Productivity represents the relationship between outputs and inputs in the production process. Improving productivity leads to the growth of wealth in the economy and ultimately to society's well-being (25).
Engineers view productivity promotion as doing the most work at the lowest cost, while scientists define productivity promotion as doing the work wisely, and at the same time, managing productivity means achieving everything together. Ultimately, economists define productivity promotion as a more productive use of available resources (26).
As one of the most important parts of the government body, the health sector can play a key role in public sector productivity. Thornhill (2006) considers productivity in the public sector important for the following reasons: 1) The major part of employment is by the public system. 2) The government is the most important provider of services that affects the cost of inputs and the quality of firms' workforce. 3) The government consumes tax resources. Therefore, the productivity of the government body can affect the productivity of the economy (27-29).
Productivity in government services are divided into four categories:
In some scientific literature, productivity is defined as the sum of its effectiveness and efficiency, and thus defines productivity as a situation whereby the system can achieve all its goals through optimal use of resources. In the health sector, productivity refers to the fact of how efficiently resources are used to achieve effectiveness (31). McKee and Figueras (2012) presented indicators such as labor productivity, the cost-effectiveness of interventions, technical efficiency, and allocative efficiency to measure health system productivity. Table 1 lists the productivity matrix based on two measures of effectiveness and efficiency. According to this matrix, although the Kali health sector production was less than the targeted program, it was produced with optimum use of resources. In other words, the health sector has been efficient, but it has not been fully effective (31). Various modes of combining efficiency and effectiveness have been shown in the productivity matrix (23). In health economics literature, a concept called cost-effectiveness is used to guarantee health sector policies' efficiency. Based on this method, the productivity of different programs is measured and compared by comparing costs and their effectiveness. Finally, the most cost-effective project is identified as the most productive option (23).
Picture of Health Sector Productivity Status
Due to restrictions on access to data on the inputs and outputs of the country's health system, this section presents an overview of the health system's productivity for measuring system output from the added-value index and total output, and the number of beds and workforce used to measure inputs. Although other factors and inputs play an important role in the output level of the health sector, there was no access to relevant data in this study. In recent years, the high costs of producing health services have led to an increase in tariffs and service prices, which has resulted in rising inflation in the health sector and consequently rising production costs. Figure 1 displays a comparison of inflation in the health sector and general inflation in the country. It also shows that inflation in the health sector has grown alongside general inflation.
Besides, the high cost of health services and the restriction of health financing from the public budget have made people's payout of 2014 much higher than the amount set out in the Fifth National Development Plan (Figure 2).
The coherent movement of the percentages of people's out of pocket payments and health sector inflation in Figure 3 is evidence of the fact that households bore the burden of inflation on the health sector.
Figure 4 presents the total production trend and the added-value of the health sector from 1992 to 2012 in billion Iranian Rials. As noticeable, the total output and added-value of the health system has been rising since 2007
but has declined steadily since then. This figure also shows that the output of the health sector is relatively stable and not significantly fluctuating.
Figure 5 discloses the growth rate of the entire health system's output. Unfortunately, the growth rate for the health sector has been declining for two decades since 1991, and in 2010 this index stands at almost zero.
Figure 6 reveals the number of beds in the country, and Figure 7 explains the number of beds increased from 1992 to 2013. According to this figure, in 2008, the number of beds in the health system has grown at a gentle slope. In 2009, there was a slight decrease in the number of beds. This decline was more severe between 2010 and 2011. After 2011, the number of beds has risen again.
Figure 8 shows the number of doctors from 1991 to 2010. Unlike the number of beds, the number of doctors has increased in an almost linear trend. In this section, the productivity of the health system is illustrated by two general system inputs: capital (bed, and labor (physician) (32). Figure 9 presents the capital productivity growth of the health system from 1991 to 2012. As visible, the trend of productivity growth has been extremely lively. The highest bed productivity growth was in 2007, at about 17 %. Later the same year, bed productivity growth had fallen to a negative 4 %. Once again, bed productivity growth was negative in 2007 and reached a negative 13 % in 2011.
Figure 10 reports the productivity growth of the physician's input from 1992 to 2012. Once more, the highest productivity growth occurred in 1993, at the frontier of 23%. At the end of the year, there was a sharp decline in physician productivity growth. Physician productivity growth was zero in 2000, negative at 7 in the year 2007, and negative at 12 % in 2012.
Generally, several factors have been suggested increasing public sector expenses and pressure on the public budget (3, 4). Similarly, the health sector as an industry that converts inputs into products in the form of health services and goods must operate efficiently and be at the frontier of its production capabilities (5).
The issue of efficiency and productivity in the health sector is important both at the micro-level such as hospitals, and at the macro level, i.e., the whole health system. The importance of productivity in the economy and the country is well reflected in the policies of a resistive economy. The newest growth models are also the sole catalyst for sustainable economic growth in productivity growth. Based on classical microeconomic models, the point where the average production curve of a firm is maximized, the mean cost curve of the variable production is minimized, and at the point where the final cost of production is minimized, the final output is maximized (6).
Therefore, it is clear that efficiency and productivity play a key role in controlling costs, especially for firms such as hospitals. So far, no similar study has been conducted on the examination and analysis of health productiveness in the country, and most of the research work in this field has investigated and analyzed the efficiency of the health system at a micro-level (hospitals and healthcare centers). These include the studies of Azar, Hoseini Nassab, Sabagh Kermani, Karimi, Fattahi, Pirani, Kiani for efficiency and situational analysis of Rezapour's health system allocation and Ahmadi's inflation indicators in the health system (7-12). Moreover, related external studies include Atella and Färe, Roberts on productivity, Ancarani, Alin O, Marieta, Eling and Kirigia, Al-Shayea, and Chan on efficiency (9, 13-20). However, in some studies on health system productivity in developed countries, the average productivity growth is mentioned as about one percent annually.
They were quite different from the present study in terms of method and did not even provide a conceptual explanation of the subject. Hence, the present study is unique in this respect. Low productivity and, therefore, higher health costs can have various problems for society and the well-being of individuals. The first effect of the high cost of production in the health sector is hospitals and health centers' declination into a cost-inflation spiral (2).
Therefore, productivity and efficiency are some of the most fundamental areas in
the scientific environment of the country. Accordingly, in this article, the authors intend to illustrate the country's health system's efficiency and effectiveness. Due to restrictions on access to data on the inputs and outputs of the country's health system, this section presents a picture of the health system's efficiency for measuring the system's output from the added-value index and total output in addition to measuring inputs. The number of beds and the workforce has been used. Although other factors and inputs also play an important role in the output of the health sector, no relevant data were available in this study. For this purpose, this article is arranged into several sections. The first section provides an overview of the concepts of productivity. The second part discloses the efficiency and productivity of the country's health system. The final section discusses the reasons for the low productivity in the health sector, its impact on key performance indicators, and offers ways to improve productivity and reduce the costs of producing health services.
Materials and Methods
Study design and literature review
This was a descriptive-analytical study in which the concept of productivity was presented in the review section using specific keywords related to the concept of productivity and searching related internal and external texts in databases. Thus, the title and abstract of all Persian and English language articles from 2000 to 2019 were extracted and screened using valid search engines such as Science Direct, Scopus, Pubmed, Magiran, Irandoc, SID, Google, scholar, Medline, and Embase Cochrane databases. At first, a large search was conducted on the Google database with high sensitivity, and later the search was conducted using proprietary strategies of each database. Keywords related to the concept of productivity, such as productivity, effectiveness, efficiency, added-value index, total output, total production, bed inpatient, manpower, workforce, and labor were used to increase the adequacy of the samples. A list of articles and books was also searched using the same keywords. Other words such as "health system," "health policy," "health sector," "health care system," "inflation" were added to the search strategy to facilitate the search process. Qualitative studies were also reviewed in this screening. Initial screening of search results by title and abstract of studies was performed by one of the browsers, the second browser independently reviewed the studies found, and the consensus was reached in cases where there was disagreement. Overall, in the first stage, about 1050 studies were initially evaluated, from which 110 studies were purposefully selected and reviewed in the second stage. Texts that had more conceptual richness (referring to the definition and interpretation of productivity concepts and other related frontiers in the field, opposing, and similar concepts and their constructs), more recent sources, authoritative journals or databases, and valid references were the criteria considered to prioritize studies (21, 22). Resources explaining the concept of productivity in other areas were excluded from the studies. Accordingly, the studies were ranked and studied in order, and finally, 20 articles were eligible for inclusion in the study, which was in full relation to the subject under study.
Total production is the maximum amount of product that can be produced with any given combination of variable and fixed inputs. On the other hand, value-added in simple language is the difference between output and input. As most scientific literature has revealed, the most practical way to measure the productivity of a system is to calculate the ratio of output (total production and value-added) to input (bed and physician) annually. In the current study, this relationship was used to extract physicians and beds' productivity in the health sector. Finally, all data from articles were extracted and screened.
Data sources and analysis
In the descriptive section, information regarding the statistical center of the Islamic Republic of Iran, the microeconomic and macroeconomic indices of health and productivity of the health sector from 1991/2 to 2011/2 were presented graphically and analyzed with the help of Excel software. Data after 2012 was not available.
The authors declare that they have complied with the principles of the Helsinki Declaration.
Results
Productivity concept
Productivity is defined as the power of production and being productive (23). In the private and commercial sectors, productivity is measured by factors such as product quality, resource effectiveness, and customer satisfaction (24). Productivity represents the relationship between outputs and inputs in the production process. Improving productivity leads to the growth of wealth in the economy and ultimately to society's well-being (25).
Engineers view productivity promotion as doing the most work at the lowest cost, while scientists define productivity promotion as doing the work wisely, and at the same time, managing productivity means achieving everything together. Ultimately, economists define productivity promotion as a more productive use of available resources (26).
As one of the most important parts of the government body, the health sector can play a key role in public sector productivity. Thornhill (2006) considers productivity in the public sector important for the following reasons: 1) The major part of employment is by the public system. 2) The government is the most important provider of services that affects the cost of inputs and the quality of firms' workforce. 3) The government consumes tax resources. Therefore, the productivity of the government body can affect the productivity of the economy (27-29).
Productivity in government services are divided into four categories:
- Productivity at the staff level
- Productivity at the organization level
- Productivity at the sector level
- Productivity at the national staff level (23).
In some scientific literature, productivity is defined as the sum of its effectiveness and efficiency, and thus defines productivity as a situation whereby the system can achieve all its goals through optimal use of resources. In the health sector, productivity refers to the fact of how efficiently resources are used to achieve effectiveness (31). McKee and Figueras (2012) presented indicators such as labor productivity, the cost-effectiveness of interventions, technical efficiency, and allocative efficiency to measure health system productivity. Table 1 lists the productivity matrix based on two measures of effectiveness and efficiency. According to this matrix, although the Kali health sector production was less than the targeted program, it was produced with optimum use of resources. In other words, the health sector has been efficient, but it has not been fully effective (31). Various modes of combining efficiency and effectiveness have been shown in the productivity matrix (23). In health economics literature, a concept called cost-effectiveness is used to guarantee health sector policies' efficiency. Based on this method, the productivity of different programs is measured and compared by comparing costs and their effectiveness. Finally, the most cost-effective project is identified as the most productive option (23).
Picture of Health Sector Productivity Status
Due to restrictions on access to data on the inputs and outputs of the country's health system, this section presents an overview of the health system's productivity for measuring system output from the added-value index and total output, and the number of beds and workforce used to measure inputs. Although other factors and inputs play an important role in the output level of the health sector, there was no access to relevant data in this study. In recent years, the high costs of producing health services have led to an increase in tariffs and service prices, which has resulted in rising inflation in the health sector and consequently rising production costs. Figure 1 displays a comparison of inflation in the health sector and general inflation in the country. It also shows that inflation in the health sector has grown alongside general inflation.
Besides, the high cost of health services and the restriction of health financing from the public budget have made people's payout of 2014 much higher than the amount set out in the Fifth National Development Plan (Figure 2).
The coherent movement of the percentages of people's out of pocket payments and health sector inflation in Figure 3 is evidence of the fact that households bore the burden of inflation on the health sector.
Figure 4 presents the total production trend and the added-value of the health sector from 1992 to 2012 in billion Iranian Rials. As noticeable, the total output and added-value of the health system has been rising since 2007
but has declined steadily since then. This figure also shows that the output of the health sector is relatively stable and not significantly fluctuating.
Figure 5 discloses the growth rate of the entire health system's output. Unfortunately, the growth rate for the health sector has been declining for two decades since 1991, and in 2010 this index stands at almost zero.
Figure 6 reveals the number of beds in the country, and Figure 7 explains the number of beds increased from 1992 to 2013. According to this figure, in 2008, the number of beds in the health system has grown at a gentle slope. In 2009, there was a slight decrease in the number of beds. This decline was more severe between 2010 and 2011. After 2011, the number of beds has risen again.
Figure 8 shows the number of doctors from 1991 to 2010. Unlike the number of beds, the number of doctors has increased in an almost linear trend. In this section, the productivity of the health system is illustrated by two general system inputs: capital (bed, and labor (physician) (32). Figure 9 presents the capital productivity growth of the health system from 1991 to 2012. As visible, the trend of productivity growth has been extremely lively. The highest bed productivity growth was in 2007, at about 17 %. Later the same year, bed productivity growth had fallen to a negative 4 %. Once again, bed productivity growth was negative in 2007 and reached a negative 13 % in 2011.
Figure 10 reports the productivity growth of the physician's input from 1992 to 2012. Once more, the highest productivity growth occurred in 1993, at the frontier of 23%. At the end of the year, there was a sharp decline in physician productivity growth. Physician productivity growth was zero in 2000, negative at 7 in the year 2007, and negative at 12 % in 2012.
Table 1. Productivity Matrix
| Low Efficiency | High efficiency | |
| High Effectiveness | Wasting part of the resources | Achieving the goals through optimal use of resources |
| Low Effectiveness | non-achievement of goals and waste of scarce resources | Low achievement of goals with optimal use of resources |
Reference: Gholipor, 2015 (23)

Figure 1. Health Inflation and Public Inflation Comparison (Source: Study Findings)
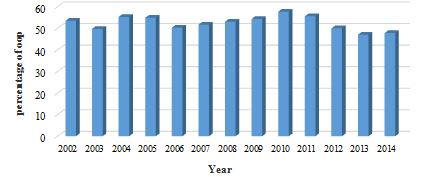
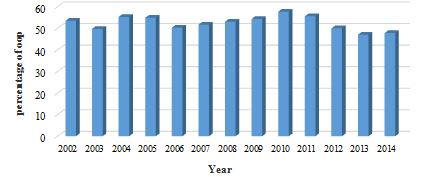
Figure 2. The Rate of People's Out of Pocket Payments (Source: Study Findings)
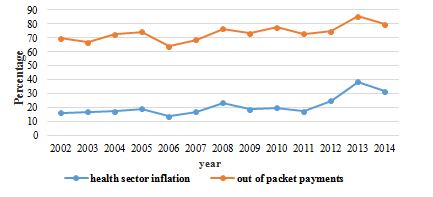
Figure 3. Concurrent Inflation of Health Sector and People's Out of Pocket Payments (Source: Study Findings)

Figure 4. Added-value and Total Health Sector Production Trend (Source: Study Findings)
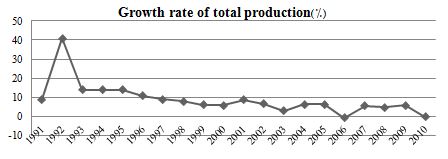
Figure 5. The Growth Rate of Total Health Sector Production (Source: Study Findings)
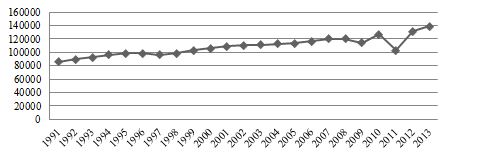
Figure 6. Bed Count Trend (Source: Study Findings)

Figure 7. The Growth rate of beds (Source: Study Findings)
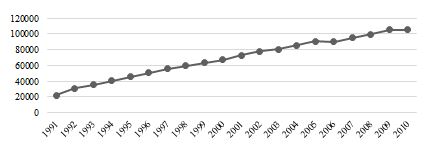
Figure 8. Trend Number of Physicians (Source: Study Findings)

Figure 9. Bed Productivity Growth Rate (Source: Study Findings)
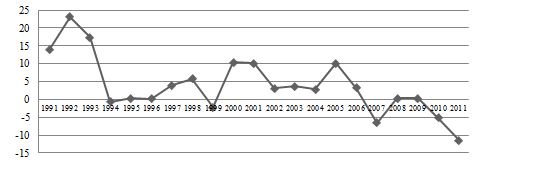
Figure 10. Physician Productivity Growth Rate (Source: Study Findings)
Discussion
As most scientific literature has shown, the most feasible way to measure a system's productivity is to calculate the input-output ratio. The current study used this relationship to derive physician and bed productivity in the health sector. The final result of this study revealed that the productivity of the health sector was not adequate. Despite the increase in the number of beds and physicians in the last two decades, the value-added and the total production of the health sector have not grown significantly. Through these terms, the authors refer to the production of the whole health sector, the real value of the total services, and marginal products produced in the health sector (33, 34).
However, this study did not judge health system performance because according to the World Health Organization report in 2000, three general indicators for measuring health system performance are outlined, i.e., the level of public health, the accountability of the health system, and protection against financial risks. The health system's performance models refer to efficiency (productivity) as an intermediate target (35, 36). Therefore, in the current research, only the efficiency and productivity of the health sector of the country are examined. Poor productivity of the country's health system can be due to various reasons. These reasons can be classified into two categories: micro and macro. In the micro sector, i.e., hospitals and healthcare centers' level, the first cause of low productivity can be attributed to the lack of full utilization of inputs. In health centers, various types of inputs such as labor, beds, medical equipment, buildings, energy, and so on are used in the service production process. If health centers are not at the frontier of utilizing these inputs, they will be inefficient in the production process and cause loss of resources. Energy is one of the factors that inefficiently utilize the production process in the health sector, especially in public health centers. In some public health centers, due to the depreciation of buildings, energy consumption is extremely high, leading to inefficiency (12, 23, 37-39).
Another reason for the low productivity in the health sector can be found in market theory. The public sector is far from market-driven. One of the characteristics of markets is that they allocate resources efficiently and exploit each resource based on its final output. This allows the density of the use of inputs in firms to be distributed efficiently and is based on maximum productivity. In government health care centers, the way that resources are combined to produce services are not market-based and is far from technical and economic measures of production. This causes the inputs not to be used according to their production capacity. Therefore, based on the findings, it can be concluded that despite the increasing number of inputs over time the output of the health sector has decreased (23, 39).
One study claims that applying different policies, even in similarly structured systems such as Italy and England, will make a difference in the efficiency of the health system. The NHS growth rate for the whole period (2004 to 2011) increased by 10 % and an average of 1.39 % per year, while overall SSN productivity increased by 5 % at an average of 0.73 % per year. Our results show that different policy goals have different outcomes for the two countries. In the UK, the NHS has focused on increasing activity, reducing waiting times, and improving quality. Contrarily, Italy is more focused on cost containment and rational provision in the hope that it will render unfair and inadequate services. The findings of this study differ from our study findings in terms of the rate of change while examining different inputs and outputs (13). At the macro level, lack of evidence-based policymaking, cross-sectoral disagreements, lack of competitive incentives in the health sector, lack of complete and transparent buyer separation from the provider, weakness of the health sector financial system, etc. are noted as factors of reduced productivity. The lack of strategic purchasing in the health sector has made the cost of services not close to their true value, and providers are demanding unrealistic tariffs and basing prices on their monopoly power, especially in the public sector. In such an environment, no health care product will have the incentive to improve productivity and reduce cost (23, 39-41). Addressing all the factors of low productivity is beyond the scope of this article. Therefore, some undesirable effects of low productivity are discussed below.
Low production efficiency (lack of optimal use of health system labor, equipment, and resources, etc.) makes the cost of health services high and causes inflation in the health sector (40, 41). In addition to this, in Iran's health system, the wage gap and price productivity have been drained due to higher wages than staff productivity. In economics, this rule is referred to as the Baumol theory. According to this theory, the growth rate of prices in an industry is equal to the difference between the growth rate of labor productivity and the growth rate of wages. The inflation of the health sector and the higher inflation of this sector of the whole economy are evidence of this phenomenon. As shown in the previous section in Figure 1, the inflation of the health sector has been higher than general inflation in recent years. The findings of Ahmadi et al. study of the years 1995 to 2007 were similar to the present research showing that the inflation of the health sector has always been higher than the public sector in Iran, but has not been a consistent trend in public and private tariffs (12). Another study in the US found that issues such as general inflation, population growth, population changes, increased per capita public health, and intensive care services have been instrumental in raising consumer prices in the health sector (42). Some other studies have reported incomplete insurance coverage and the share of people paying premiums as factors in increasing health costs (43). Other researchers believe that increasing insurance coverage will cause technological changes and ultimately increase health costs (44). Newhouse categorizes these inflation factors into two groups of demand-side that include community aging, expansion of insurance coverage, and supply-side category that consist of inducing demand, growth in productivity, and insurance companies' management and technological change (45). Therefore, higher inflation in the health sector than in the public sector has been confirmed in most of these studies. In addition to the factors mentioned earlier, factors such as the increase in the quantity and quality of hospital hotels, more specialized human resources, etc. should also be added to Iran's list (12). A study in Norwegian hospitals shows that the rate of physicians' productivity declined between 2001 and 2013, followed by health reforms. The main reason for this is the lack of the support of nursing staff and ward secretaries (46). According to the OECD productivity survey, the main reasons for the increase in Denmark and Canada's productivity are the technical changes (9). In another study for OECD countries, the main causes of inefficiency in health care were factors outside the control of the health system, including GDP, education, smoking habit, and obesity. High inflation in the health sector coupled with the lower purchasing power of the population either pushes the burden of financing rising health care spending on the public budget or increases the catastrophic health expenditure spending and out-of-pocket payments resulting in poverty from health spending. The concurrent movement of inflation in the health sector and the amount of out-of-pocket of the population shows that the inflationary pressure of the health sector in Iran has been on the rise in recent years. Low productivity can also affect the quality of health services (12, 47).
Ancarani et al. (16), in reviewing the technical efficiency of Italian hospitals, found that managerial decisions to use more resources than external factors had a greater impact on health efficiency. Gunnarsson et al. (48) have evaluated the efficacy of these costs by referring to the magnitude and importance of government health and education costs in countries. They attribute the underlying causes of countries' inefficiencies to inadequate access to real resources such as teachers and medicine and also point out that higher costs will be associated with lower efficiency. Alin O, Marieta analyzed the economic efficiency of the health system in Europe using health indicators and the ratio of health costs to GDP and concluded that the average health expenditure efficiency in the European :union: was less than one, concluding that its benefits were lower than the costs (49). A comparison of the average efficiency of public and private health expenditure in the countries of the region and North Africa (MENA) claims that the efficiency of private health expenditure has improved over the 2005- 2010 period and the gap between the efficiency of these two types of expenditure in the health sector has declined. The main reason for this is the reduction of public expenditure efficiency on the one hand and the improvement of private expenditure efficiency on the other. The lowest and highest average technical efficiency of public health expenditures were related to Jordan and Yemen, respectively. In contrast, the lowest and highest mean technical efficiency of private health expenditures is allocated to Lebanon, Mauritania, and Oman, respectively. This study continues to redefine public health expenditure, reform public health expenditure structure, revise the method of resource allocating health expenditure, and so on. On the other hand, it recommends helping improve the efficiency of private spending especially through the transfer of health units to this sector (7). Efficiency is one of the most important indicators of productivity. Measuring this index is a criterion for comparing the utilization of available resources against standard criteria or an index for assessing the performance of homogeneous and homogeneous units. The study by Rezapour et al. (50) showed that Southwest Asian countries suffer from economic inefficiencies due to the 12 % unproductivity of resources which is a result of poor efficiency of management, scale, and allocation. The study reported that the countries under investigation were able to access the same basic health indicators by using and allocating 88 % of the current health system resources. According to the World Health Organization, more than 50 % of resources in health care are inadequate (50). Robert's study (2008) of the inefficiencies of the OECD countries showed that the main reason for the weakness of productivity in health systems is the weakness in the allocation of health system resources (14). Evans (2001) attributed the inefficiency of health systems to the low cost of health care per capita. The results of some studies emphasize the role of management inefficiency (51). Good management is prominent in the health system, motivation, and effort of human resources for high-powered activity, training, and supply of human resources. The absence of a systematic assessment of the health system, lack of human resources in a position that is appropriate to their skills and education, lack of motivation for training promotion and specialization, lack of areas of creativity and variety, etc. can all affect the efficiency of human resources (8, 9). Another study does not consider the cause of low efficiency and increased costs in specialist workforce shortages but rather focuses on factors such as lack of utilization, maintenance and support, how resources are allocated at different levels, and how much they spend to improve health system performance. Overall, these studies emphasize the role and importance of managers in enhancing performance (9). Therefore, poor production makes the services provided in the health sector not of good quality and effectiveness. This may affect other health performance indicators (12).
Conclusion
In conclusion, suggestions for improving the productivity of the health sector are as follows:
- Requiring full and accurate implementation of operational budgeting in government health centers;
- Implementing performance-based management in the public health sector;
- Implementing performance-based incentive systems;
- Improving government buildings;
- Developing and implementing technical and managerial models of energy use improvement;
- Creating a healthy competition environment between health centers;
- Making policy for the management of advanced medical equipment in the health sector
- Providing competition among providers through the implementation of strategic purchasing;
- Using efficient, evidence-based manufacturing methods in health centers.
The authors thank Dr. Ahadinezhad for providing the data and the preliminary idea of the manuscript.
Conflict of interests
The authors declared that there is no conflict of interests in the present study.
Authors' contributions
Hosseini-Shokouh SM designed research; Nasiri T conducted research; Nasiri T Analyzed data; Hosseini-Shokouh SM and Nasiri T wrote manuscript. All authors read and approved the final manuscript.
Funding
Non applicable
Type of Study: Original article |
Subject:
Health Economics
Received: 2020/08/23 | Accepted: 2021/03/10 | Published: 2021/03/10
Received: 2020/08/23 | Accepted: 2021/03/10 | Published: 2021/03/10
References
1. Winch P, Stepnitz R. Peak oil and health in low-and middle-income countries: impacts and potential responses. American Journal of Public Health. 2011; 101(9): 1607-14. [DOI:10.2105/AJPH.2011.300231]
2. Assadzadeh A, Parishani M, Mansouri B. The Effects of Oil Revenue Shocks on Health Expenditures in Iran. Health Information Management. 2015; 11(7): 880-8.
3. Roberts M, Hsiao W, Berman P, Reich M. Getting health reform right: a guide to improving performance and equity: Oxford university press; 2008. [DOI:10.1093/acprof:oso/9780195371505.001.0001]
4. Bodenheimer TS, Grumbach K. Understanding health policy: A clinical approach 4 th edition: New York, NY: McGraw-Hill Companies, Inc; 2004.
5. Fique JP. Evaluating Hospital Efficiency Adjusting for Quality Indicators: an Application to Portuguese NHS Hospitals. Universidade do Porto, Faculdade de Economia do Porto; 2011.
6. Henderson JM, Quandt RE. Microeconomic theory: A mathematical approach. 1971.
7. Fattahi M, Barkhordari S. The Efficiency of Public And Private Health Expenditures: DEA Approach. Journal of Healthcare Management (Journal of Health System). 2014; 5(3): 41-51.
8. Rezapour A, Asefzadeh S. Study economic efficiency of teaching hospitals of Qazvin University of Medical Sciences (1999-2007). Journal of Guilan University of Medical Sciences. 2009; 18(71): 55-63.
9. Rezapoor A, Ebadifard Azar F. Situation of resource allocation in Iranian, s health system. Journal of Hospital. 2013; 11(4): 53-64.
10. Kiani MM, Mosavi Rigi SA, Karami H, Sepaseh F, Naghdi B, Shiravani M. Efficiency Evaluation of University Hospitals In Bushehr Province before and after the Implementation of the Health System Development Plan. Evidence Based Health Policy, Management and Economics. 2018; 2(1): 1-11.
11. Sajadi H, Karami M, Torkzadeh L, Karimi S, Bidram R. Efficiency estimation in general hospitals of Isfahan University of medical sciences during 2005-2006 by data envelopment analysis. 2009.
12. Ahmadi AM, Yousefi M, Fazaeli S. Consumer Price Index Changes in Iran's Public and Health Sectors. The Economic Reseach. 2010; 10(1): 99-111. [In Persian]
13. Atella V, Belotti F, Bojke C, Castelli A, Grašič K, Kopinska J, et al. How health policy shapes healthcare sector productivity? Evidence from Italy and UK. Health Policy. 2019; 123(1): 27-36. [DOI:10.1016/j.healthpol.2018.10.016]
14. Retzlaff-Roberts D, Chang CF, Rubin RM. Technical efficiency in the use of health care resources: a comparison of OECD countries. Health Policy. 2004; 69(1): 55-72. [DOI:10.1016/j.healthpol.2003.12.002]
15. Alin O, Marieta M. Determining the efficiency of health expenditure as a prerequisite for achieving economic equilibrium in the European :union:. Economics and Finance Research. 2011; 4: 81-5.
16. Ancarani A, Di Mauro C, Giammanco M. The impact of managerial and organizational aspects on hospital wards' efficiency: Evidence from a case study. European Journal of Operational Research. 2009; 194(1): 280-93. [DOI:10.1016/j.ejor.2007.11.046]
17. Eling M, Luhnen M. Efficiency in the international insurance industry: A cross-country comparison. Journal of Banking & Finance. 2010; 34(7): 1497-509. [DOI:10.1016/j.jbankfin.2009.08.026]
18. Kirigia JM, Asbu EZ. Technical and scale efficiency of public community hospitals in Eritrea: an exploratory study. Health Economics Review. 2013; 3(1): 6. [DOI:10.1186/2191-1991-3-6]
19. Al-Shayea AM. Measuring hospital's units efficiency: A data envelopment analysis approach. International Journal of Engineering & Technology. 2011; 11(6): 7-19.
20. Chan S-G, Karim MZA. Public spending efficiency and political and economic factors: Evidence from selected East Asian countries. Economic Annals. 2012; 57(193): 7-24. [DOI:10.2298/EKA1293007C]
21. Adib b SM, Parvisi S. Qualitative Methods. Tehran: Boshra Press; 2005. First Published in 2005.
22. Nasiri T, Takian A, Yazdani S. Stewardship in Health, Designing a Multi-Layer Meta Model: A Review Article. Iranian Journal of Public Health. 2019; 48(4): 579-92. [DOI:10.18502/ijph.v48i4.979]
23. Gholipour R. The Challenges of Productivity In Government. Journal of Public Administration. 2015; 7(3): 595-618. [In Persian]
24. Parker D, Waller K, Xu H. Private and public services: productivity and performance migration. International Journal of Productivity and Performance Management. 2013; 62(6): 652-64. [DOI:10.1108/IJPPM-10-2012-0119]
25. Iran CBotIRo. Iranian Economic Productivity Report (1988 to 2007) In: Economic Deputy EAO, editor. Iran Central Bank of the Islamic Republic of Iran. 2010. p. 1-22.
26. Nasrollahnia M, Rahmanizadeh F. Performance Evaluation of Productivity Growth and Some Member Countries of The Asian Productivity. Financial Knowledge of Security Analysis (Financial Studies). 2014; 23(7): 109-23.
27. Thornhill D. Productivity Attainment in a Diverse Public Sector, paper presented at the Institute of Public Administration Seminar on Promoting Productivity in a Diverse Public Sector, Dublin. 21 April 2006.
28. Rosiek A, Rosiek-Kryszewska A, Leksowski Ł, Kornatowski T, Leksowski K. The employee's productivity in the health care sector in Poland and their impact on the treatment process of patients undergoing elective laparoscopic cholecystectomy. Patient Preference and Adherence. 2016; 10: 2459. [DOI:10.2147/PPA.S119348]
29. Pourreza A, Alipour V, Arabloo J, Bayati M, Ahadinezhad B. Health production and determinants of health systems performance in WHO Eastern Mediterranean Region. Eastern Mediterranean Health Journal. 2017; 23(5): 368-74. doi: 10.26719/2017.23.5.368. [DOI:10.26719/2017.23.5.368]
30. Nayebi H, Ebrahimi R, Azadegan A. Measuring and Analyzing the Factors Affecting the Growth of Total Factor Productivity in Iranian Economy Using Solo Residual Method. Macroeconomic Research Journal (Journal of Economic Sciences). 2010; 10(1): 121-40.
31. McKee M, Figueras J, Saltman RB. Health systems, health, wealth and societal well-being: Assessing the case for investing In health systems: Assessing the case for investing in health systems: McGraw-Hill Education (UK); 2011.
32. Abedi G, Marvi A, Kentaie S, Amir S, Abedini E, Asadi Aliabadi M, et al. SWOT Analysis of Implementation of Urban Family Physician Plan from the Perspective of Beneficiaries: A Qualitative Study. Journal of Mazandaran University of Medical Sciences. 2017; 27(155): 79-93. [In Persian]
33. Khezrimotlagh D, Chen Y. The Ratio of Output to Input Factors. Decision Making and Performance Evaluation Using Data Envelopment Analysis. Cham: Springer International Publishing; 2018. p. 235-50. [DOI:10.1007/978-3-319-76345-3_8]
34. Kao C. Output-Input Ratio Efficiency Measures. Network Data Envelopment Analysis: Foundations and Extensions. Cham: Springer International Publishing; 2017. p. 19-41. [DOI:10.1007/978-3-319-31718-2_2]
35. Organization WH. The world health report 2000: health systems: improving performance: World Health Organization; 2000.
36. Shams L, Akbari Sari A, Yazdani S. Values in Health Policy - A Concept Analysis. International Journal of Health Policy and Management. 2016; 5(11): 623-30. [DOI:10.15171/ijhpm.2016.102]
37. Nabilou B, Yusefzadeh H, Rezapour A, Azar FEF, Safi PS, Asiabar AS, et al. The productivity and its barriers in public hospitals: case study of Iran. Medical journal of the Islamic Republic of Iran. 2016; 30: 316.
38. Moosazadeh M, Amiresmaili MR. Study of productivity status and related factors and determining at selected hospitals of Mazandaran province- 2010. Tolooe Behdasht. 2012; 10(1):1-13.
39. Iran CBotIRo. Iranian Economic Productivity Report 2001 to 2009. In: Deputy E, editor. Economic Accounts Office; 2010. p. 1-22.
40. Branson WH. Macroeconomic theory and policy. 1979.
41. Snowdon B, Vane HR, Wynarczyk P. A modern guide to macroeconomics. Books. 1994.
42. Rosko MD, Broyles RW. The economics of health care: a reference handbook. 1988.
43. Warshawsky MJ. Factors contributing to rapid growth in national expenditures on health care. Trends in Health Benefits. 1993: 65.
44. Weisbrod BA. The health care quadrilemma: an essay on technological change, insurance, quality of care, and cost containment. Journal of Economic Literature. 1991; 29(2): 523-52.
45. Newhouse JP. Medical care costs: how much welfare loss?. Journal of Economic Perspectives. 1992; 6(3): 3-21. [DOI:10.1257/jep.6.3.3]
46. Johannessen KA, Kittelsen SA, Hagen TP. Assessing physician productivity following Norwegian hospital reform: A panel and data envelopment analysis. Social Science & Medicine. 2017; 175: 117-26. [DOI:10.1016/j.socscimed.2017.01.008]
47. Baumol WJ, Blinder AS. Microeconomics: Principles and policy: Nelson Education; 2015.
48. Gunnarsson V, Carcillo S, Verhoeven M. Education and health in G7 countries: Achieving better outcomes with less spending: International Monetary Fund; 2007. [DOI:10.5089/9781451868265.001]
49. Alin O MM. determining the efficiency of health expenditure as a prerequisite for achieving economic equilibrium in the European :union:. International Conference on Economics and Finance Research. 2011.
50. Organization WH. World Health Report 2000. Health Systems: Improving Performance. Geneva: World Health Organization; 2000 [Citado 13 Abr 2013].
51. Evans DB, Tandon A, Murray CJ, Lauer JA. Comparative efficiency of national health systems: cross national econometric analysis. Bmj. 2001; 323(7308): 307-10. [DOI:10.1136/bmj.323.7308.307]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |