Volume 5, Issue 3 (10-2021)
EBHPME 2021, 5(3): 176-184 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Mohammadi F, Masoudi Asl I, Mahfoozpour S, Hessam S. Factors Affecting Hospital Network Management in the Social Security Organization of Iran. EBHPME 2021; 5 (3) :176-184
URL: http://jebhpme.ssu.ac.ir/article-1-335-en.html
URL: http://jebhpme.ssu.ac.ir/article-1-335-en.html
Department of Health Services Management, School of Health Management and Information Sciences, Iran University of Medical Sciences, Tehran, Iran , drmasoudiasl@gmail.com
Full-Text [PDF 1429 kb]
(554 Downloads)
| Abstract (HTML) (1469 Views)
Full-Text: (189 Views)
Background: Hospitals are considered the most important consumer units in the health system. Based on the effect of the hospital network in optimal and efficient hospital management, this study aimed to identify and explain the role of factors influencing hospital network management in the Iranian Social Security Organization (ISSO).
Methods: This study was conducted by a mixed method in 2018. First, variables and factors affecting the management of hospital networks were extracted from the literature review and through interviews with 15 experts, and a questionnaire with 40 questions was developed. Then, it was distributed among 448 experts in the healthcare section of the ISSO all over the country, and 405 questionnaires were completed and collected. Data were analyzed via exploratory and confirmatory factor analysis and structural equations using SPSS23 software and AMOS24 software. The validity of the questionnaire was determined via expert judgment (CVRs = 0.40) and reliability was estimated by Cronbach's alpha coefficient (α = 0.87).
Results: Based on the confirmatory factor analysis, financing, monitoring and evaluation, accountability, strategic planning, and decision rights were identified as key factors affecting hospital network management. Financing with standard coefficients of 0.83 had the highest and decision rights with standard coefficients of 0.44 had the lowest effect on hospital network management of the ISSO.
Conclusion: To efficient hospital network management of the ISSO, while emphasizing all identified factors, special attention should be paid to financing and modifying the method of budgeting and using suitable monitoring and evaluation mechanisms.
Key words: Hospital network, Management, Health system
The healthcare reform in Norway was started to promote the efficiency of hospitals and improve the quality of healthcare services. This reform was included granting decision rights to the healthcare system in financing, administration and staff recruitment, dismiss and transfer. The accent of these reforms was on the necessity for improvement of healthcare management (7). A Survey of reforms in the public hospitals of some countries indicated that the health ministry interferes in selecting healthcare staff and allocated hospital equipment. Also, the budget and expenses of hospitals are governed by the ministry of economy and finance consequently, hospitals cannot be completely autonomous without decision rights over their staff, revenue, and expenses (8, 9).
Establishing health care companies and granting authority hospitals, decision rights in human resources management are devolved to these companies' board of directors (10). Also, the use of the corporate structure in health care management creates opportunities for reorganizing services, increasing investment and revenues, and improving wages for employees. Hence, it results in increased efficiency and effectiveness of health care management (11, 12).
Some countries launched hospital networks. A hospital network is an emerging organizational form designed to face the new challenges of healthcare systems that provide two or more hospitals and other broad healthcare facilities and services (13, 14). In Spain and Estonia, with the launch of the hospital network, decision rights improved, and clear responsibility and obvious financial management were achieved. Also, the restructured hospitals demonstrated higher efficiency and lower production costs than control facilities; in addition, operating deficits also obviously decreased (15, 16). The hospital network had the added advantage of placing most services in a multihospital network under a single management structure. This resulted in the integration of facilities and led to efficiency gains by reducing underutilized infrastructure, merging specialty and hospital services, and centralizing support and diagnostic functions such as information technology and laboratory services. The healthcare reforms were accompanied by introducing a diagnosis-related group (DRG) payment mechanism for hospitals. Cost inhibition results have been significant; once the reforms were in place, annual cost increases were more than halved (17).
ISSO, which has been considered one of the healthcare services providers in the country with 294 outpatient centers and 76 hospitals, provides healthcare services to about 42,000,000 people (18). Now, ISSO's hospitals face challenges, including an unsuitable organizational structure, lack of decision rights in budgeting and human resources, the deficit of liquidity, and growth of healthcare services expenditure. This demonstrates the importance of organizational reform and modification of hospital management (19). Based on the effect of the hospital network in optimal and efficient hospital management, this study aimed to identify and explain the role of factors influencing hospital network management in the ISSO.
Materials and Methods
This study was conducted by a mixed method in 2018 in 2 phases (qualitative-quantitative) as follows:
The qualitative phase: In this phase, First, variables and factors affecting the management of hospital network were extracted from the literature review (books, journals, documents, reports, scientific papers, search engine such as Irandoc, Medline, PubMed, Scopus, Elsevier) and through interview with 15 experts in the field of healthcare management. The entry criterion for experts was a minimum experience of 10 years in health services or hospital administration positions. The interviews were recorded and transcribed according to the permission of experts. The data obtained from this stage were categorized, and redundant data were removed. The most significant variable influencing the management of hospital networks were classified into five groups and 40 components.
The quantitative phase: Based on the data obtained from the previous phase, a questionnaire rated on a Likert scale was developed. The validity of the questionnaire was determined via expert judgment. The coefficients of variation ratio (CVRs) were higher than the critical level (0.49), which is acceptable. After confirming the content and face validity of the questionnaire, to define the reliability of the questionnaire, Cronbach's alpha was estimated using SPSS23 software, and its internal consistency was approved (α = 0.87).
The statistical population was composed of directors and experts in healthcare management in the healthcare section of the ISSO all over the country. Using the Cochran formula, the sample size was determined. The questionnaires were distributed to 448 experts, and 405 questionnaires were completed and gathered (90.40 %). The Kaiser-Meyer-Olkin (KMO) method was used to determine the sufficiency of sample size, and Bartlett's test of sphericity was used to determine whether the correlation matrix differs from zero or not. Data were analyzed using SPSS23 software. Factors influencing hospital network management of the ISSO were extracted and approved via exploratory and confirmatory factor analysis with structural equation modeling approach in AMOS24 software. The authors have completely observed ethical issues (Including plagiarism, informed consent, misconduct, data fabrication, double publication and submission, redundancy, etc.). The thesis code is 14121213962026. It should be noted that this study tried to comply with the principles of the Helsinki Declaration.
Results
According to our literature review and interviews, the most important variables influencing the management of hospital network were classified into five groups of strategic planning factors (6 components), decision rights factors (11 components), financing factors (7 components), monitoring and evaluation factors (7 components), and accountability factors (9 components).
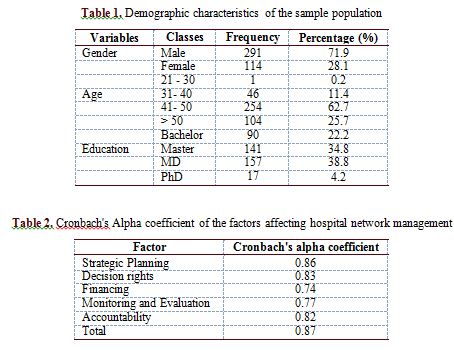
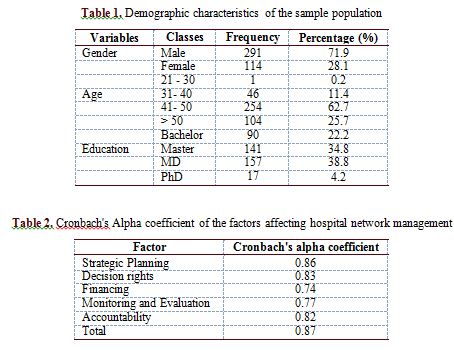
In this research, of the 448 questionnaires distributed, 405 questionnaires (90.40 %) were completed and analyzed. Among the experts, there were 291 men (71.90 %) and 114 women ( 28.10 %). Most of them, aged between 41 and 50 years (62.70 %), with MD education (38.80 %). The demographic characteristics of the sample population are presented in Table 1.
The reliability of the questionnaire was calculated using Cronbach's alpha coefficient, and its internal consistency was approved (Cronbach's alpha = 0.87). Also, the internal consistency of the 5 areas, including strategic planning factors, decision rights factors, financing factors, monitoring and evaluation factors, and accountability factors, were approved. The details for each factor are presented in Table 2.
The sufficiency of sample size was calculated at 0.87 using the KMO index. Further, Bartlett's test of sphericity (6870), which is significant at an error level (0.001), indicates a proper correlation between the items in each factor. The findings of exploratory factor analysis, using the Varimax rotation, revealed five key factors with Eigenvalues more than one remained in the analysis. These factors could explain 71.64 % of the total variance in the variables. The Eigenvalues of factors affecting hospital network management are presented in Table 3.
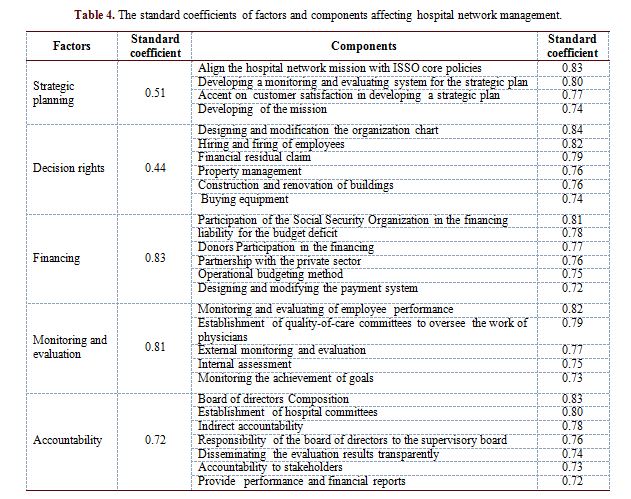
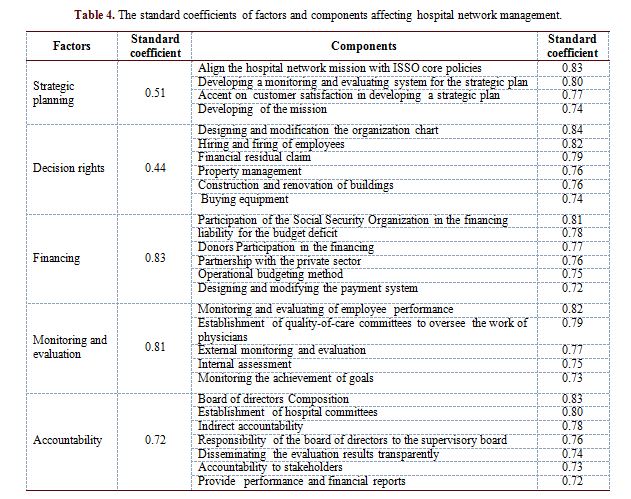
After exploratory factor analysis, confirmatory factor analysis confirmed the five key factors and 28 components affecting hospital network management, including strategic planning factors (4 components), decision rights factors (6 components), financing factors (6 components), monitoring and evaluation factors (5 components), and accountability factors (7 components), that significant correlation witnessed among them. The most and least factor loadings were assigned to financing and decision rights, with standard coefficients of 0.83 and 0.44, respectively.
In the assessment of components of the strategic planning factor, it was found that the component of the alignment of the hospital network mission with the major policies of the ISSO with standard coefficients of 0.83 had the most influence and component of the formulation of the mission with standard coefficients of 0.74, has the lowest influence at strategic planning. Also, in the decision rights factor, designing and revising the organization chart and purchasing equipment with standard coefficients of 0.84 and 0.74 had the most and least influence, respectively.
The highest and lowest influence components in the financing factor were participation of the Social Security organization in the financing and designing and changing the payment system with standard coefficients of 0.81 and 0.72, respectively. In monitoring and evaluation, the component of monitoring and evaluating of staff performance had the most influence with standard coefficients of 0.82, and the component of monitoring the achievement of goals with standard coefficients of 0.73 had the least influence. The highest and lowest influence components in the accountability factor were the Composition of the board of directors and the presentation of functional and financial reports with standard coefficients of 0.83 and 0.72, respectively. Table 4 demonstrates the standard coefficients of factors and components affecting hospital network management.
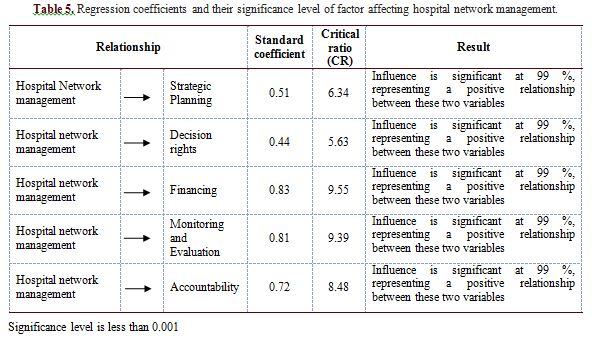
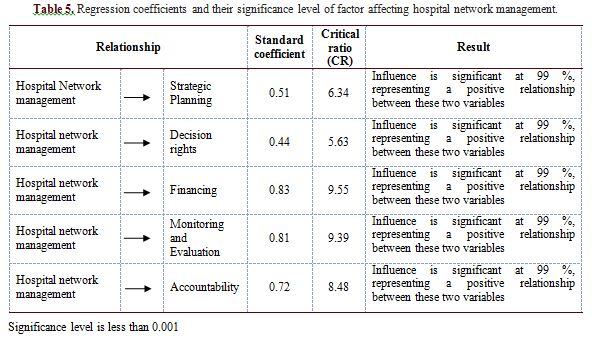
Results of research hypotheses testing, regression coefficients, and significance level of structural model are presented in Table 5. As shown, an overview of relationships between variables indicates that all the relationships are confirmed.

In a study by Duran and Salman, factors of institutional arrangements, financing, accountability, and decision rights capacity against responsibility were explained as the main factors of hospital management (4). Also, Nasiripour et al. (10), in a research in 2007, proposed a pattern for corporative hospital management. This pattern included the main factors of decision rights, residual claimant status, market exposure, accountability, and social responsibilities. These findings are consistent with the results of the current research.
According to the results of current research, strategic planning, monitoring the achievement of goals, monitoring and evaluating of employee performance, establishment of quality-of-care committees to oversee the work of physicians, decision rights in construction and repair of buildings, and equipment purchase, are factors affecting the management of hospital network, which warrant our attention. This finding is consistent with Alexander and Schroer's findings in 1985 (20), Dolci et al. (21), Jones et al. (22), and Jackson et al. (23).
The results of the study by Alexander and Schroer in 1985 showed that in the hospital network, most decisions are related to medical staff privileges, adding and removing services at the hospital level, hospital strategic planning, operational and capital budgets, evaluating the hospital CEO's performance, and and appointing the hospital CEO (20). Dolci et al. (21), conducted a study in 2011 to identify the conformity of the objectives of the medical units, the analysis of the efficiency and utilization of resources, the alignment of the mission and values of the organization, the quality and safety standards of the patient, and the degree of coordination between medical units and the health system as a whole. They suggest an evaluation system for specialized hospitals by monitoring performance indicators. Jones et al. (22), in 2017, and Jackson et al. (23), in 2007, also concluded that strategic planning, the systematic development and updating of the` vision, mission, goals, setting of short-term and long-term priorities, and regular evaluation of the functions, are the main factors influencing the management of healthcare organizations.
According to the results of current research, one of the main factors in hospital network management is accountability, which is consistent with the results of the study by Aghazade (6), in 2012 Lewis and Pettersson (24), in 2009 and Lemière et al. (25), in 2012. These researchers believe that the lack of execution of suitable accountability mechanisms in hospitals is one of the major reasons for failure in reforms of hospitals.
The results of this research demonstrated that financing is the most important factor influencing the management of hospital networks. In a study by Kutzin et al. (1), those countries they raised as successful reformers changed away from major health system structural reforms to designing and implementing a coherent and well- functioning health financing system, which is consistent with the results of this study.
According to the current research results, modifying budgeting methods and using operational budgeting methods is one of the important components in hospital network management. This finding is consistent with the findings of researches by Duran and Salman in 2013, La Forgia and Couttolenc in 2008, and Dolci et al. (4, 17, 21) in 2011. Further, the findings of this study showed that the hospital's responsibility against the probable deficiencies can be effective in hospital management, which is consistent with the results of the study by Nasiripour et al. (10), in 2007 and Lemière et al. (25), in 2012.
The findings of the present study demonstrated that decision rights in staff recruitment and dismiss, are one of the main factors in the improvement of hospital network management. Based on the research by De Geyndt in 2017 and La Forgia and Couttolenc in 2008, decision rights to staff recruitment, dismissal, promotion, and transfer can lead to an improvement in the hospitals' performance (8, 17), which is consistent with the results of the present study. In this regard, the findings of a research by Pettersen et al. (7) in 2012 indicated that extensive area for decision making in staff recruitment and dismissal might raise problems such as ambiguity and opportunism for the boards, which is inconsistent with this research.
This research had some limitations. Inclusion criteria were used for the interviewees, so some experts may have been left out. If the participants had changed, our findings would have been different. However, the strength of this study was its global design and including ISSO hospitals across the country.
Conclusion
This study specified factors affecting the management of hospital networks. Considering the exigency to modify and improve the management of ISSO's hospitals and based on the present study, it seems that policymakers and managers of social security organization hospitals should pay more attention to human resources management, financing, using operational budgeting methods, payment systems, property management, monitoring, and evaluation systems, using suitable accountability mechanism and accent on customer satisfaction in developing a strategic plan. The findings of the current research can be used to manage public and private hospitals and other healthcare organizations.
Acknowledgments
The authors would like to thank the ISSO experts for their assistance in the data collection process.
Conflict of interests
The authors declared no conflict of interests.
Authors' contributions
Mohammadi F, Masoudi Asl I, Mahfoozpour S and Hessam S designed research; Masoudi Asl I, Mahfoozpour S and Mohammadi F conducted research; Hessam S analyzed data; and Mohammadi F, Masoudi Asl I and Mahfoozpour S wrote the paper. Masoudi Asl I had primary responsibility for final content. All authors read and approved the final manuscript.
Funding
It was not financially supported.
Methods: This study was conducted by a mixed method in 2018. First, variables and factors affecting the management of hospital networks were extracted from the literature review and through interviews with 15 experts, and a questionnaire with 40 questions was developed. Then, it was distributed among 448 experts in the healthcare section of the ISSO all over the country, and 405 questionnaires were completed and collected. Data were analyzed via exploratory and confirmatory factor analysis and structural equations using SPSS23 software and AMOS24 software. The validity of the questionnaire was determined via expert judgment (CVRs = 0.40) and reliability was estimated by Cronbach's alpha coefficient (α = 0.87).
Results: Based on the confirmatory factor analysis, financing, monitoring and evaluation, accountability, strategic planning, and decision rights were identified as key factors affecting hospital network management. Financing with standard coefficients of 0.83 had the highest and decision rights with standard coefficients of 0.44 had the lowest effect on hospital network management of the ISSO.
Conclusion: To efficient hospital network management of the ISSO, while emphasizing all identified factors, special attention should be paid to financing and modifying the method of budgeting and using suitable monitoring and evaluation mechanisms.
Key words: Hospital network, Management, Health system
Introduction
| Policymakers in most countries, especially developing countries, face the challenge of improving the performance of their healthcare systems (1). Hospitals are considered the most important consumer units in the health system and one of the principal organizations of healthcare services (2). Therefore, the need for evaluation of their performance and efficient management is inevitable (3). Overuse of resources, the increasing patient expectancy of services quality and selection of healthcare providers, and enhanced political pressure for modifying the management structure are among factors that lead to healthcare management changes (4). Healthcare reforms depend on the consonances of healthcare strategies, their performance, and supervision of their managers (5). In research on reforms at healthcare system of the countries including Canada, Sweden, Chile, Mexico, Western Europe, Latin America, and the United Kingdom, the factors of responsibility, accountability, monitoring and evaluation, and improvement of performance were mentioned as the major pillars of organizational reforms at health sector (6). |
Establishing health care companies and granting authority hospitals, decision rights in human resources management are devolved to these companies' board of directors (10). Also, the use of the corporate structure in health care management creates opportunities for reorganizing services, increasing investment and revenues, and improving wages for employees. Hence, it results in increased efficiency and effectiveness of health care management (11, 12).
Some countries launched hospital networks. A hospital network is an emerging organizational form designed to face the new challenges of healthcare systems that provide two or more hospitals and other broad healthcare facilities and services (13, 14). In Spain and Estonia, with the launch of the hospital network, decision rights improved, and clear responsibility and obvious financial management were achieved. Also, the restructured hospitals demonstrated higher efficiency and lower production costs than control facilities; in addition, operating deficits also obviously decreased (15, 16). The hospital network had the added advantage of placing most services in a multihospital network under a single management structure. This resulted in the integration of facilities and led to efficiency gains by reducing underutilized infrastructure, merging specialty and hospital services, and centralizing support and diagnostic functions such as information technology and laboratory services. The healthcare reforms were accompanied by introducing a diagnosis-related group (DRG) payment mechanism for hospitals. Cost inhibition results have been significant; once the reforms were in place, annual cost increases were more than halved (17).
ISSO, which has been considered one of the healthcare services providers in the country with 294 outpatient centers and 76 hospitals, provides healthcare services to about 42,000,000 people (18). Now, ISSO's hospitals face challenges, including an unsuitable organizational structure, lack of decision rights in budgeting and human resources, the deficit of liquidity, and growth of healthcare services expenditure. This demonstrates the importance of organizational reform and modification of hospital management (19). Based on the effect of the hospital network in optimal and efficient hospital management, this study aimed to identify and explain the role of factors influencing hospital network management in the ISSO.
Materials and Methods
This study was conducted by a mixed method in 2018 in 2 phases (qualitative-quantitative) as follows:
The qualitative phase: In this phase, First, variables and factors affecting the management of hospital network were extracted from the literature review (books, journals, documents, reports, scientific papers, search engine such as Irandoc, Medline, PubMed, Scopus, Elsevier) and through interview with 15 experts in the field of healthcare management. The entry criterion for experts was a minimum experience of 10 years in health services or hospital administration positions. The interviews were recorded and transcribed according to the permission of experts. The data obtained from this stage were categorized, and redundant data were removed. The most significant variable influencing the management of hospital networks were classified into five groups and 40 components.
The quantitative phase: Based on the data obtained from the previous phase, a questionnaire rated on a Likert scale was developed. The validity of the questionnaire was determined via expert judgment. The coefficients of variation ratio (CVRs) were higher than the critical level (0.49), which is acceptable. After confirming the content and face validity of the questionnaire, to define the reliability of the questionnaire, Cronbach's alpha was estimated using SPSS23 software, and its internal consistency was approved (α = 0.87).
The statistical population was composed of directors and experts in healthcare management in the healthcare section of the ISSO all over the country. Using the Cochran formula, the sample size was determined. The questionnaires were distributed to 448 experts, and 405 questionnaires were completed and gathered (90.40 %). The Kaiser-Meyer-Olkin (KMO) method was used to determine the sufficiency of sample size, and Bartlett's test of sphericity was used to determine whether the correlation matrix differs from zero or not. Data were analyzed using SPSS23 software. Factors influencing hospital network management of the ISSO were extracted and approved via exploratory and confirmatory factor analysis with structural equation modeling approach in AMOS24 software. The authors have completely observed ethical issues (Including plagiarism, informed consent, misconduct, data fabrication, double publication and submission, redundancy, etc.). The thesis code is 14121213962026. It should be noted that this study tried to comply with the principles of the Helsinki Declaration.
Results
According to our literature review and interviews, the most important variables influencing the management of hospital network were classified into five groups of strategic planning factors (6 components), decision rights factors (11 components), financing factors (7 components), monitoring and evaluation factors (7 components), and accountability factors (9 components).
In this research, of the 448 questionnaires distributed, 405 questionnaires (90.40 %) were completed and analyzed. Among the experts, there were 291 men (71.90 %) and 114 women ( 28.10 %). Most of them, aged between 41 and 50 years (62.70 %), with MD education (38.80 %). The demographic characteristics of the sample population are presented in Table 1.
The reliability of the questionnaire was calculated using Cronbach's alpha coefficient, and its internal consistency was approved (Cronbach's alpha = 0.87). Also, the internal consistency of the 5 areas, including strategic planning factors, decision rights factors, financing factors, monitoring and evaluation factors, and accountability factors, were approved. The details for each factor are presented in Table 2.
The sufficiency of sample size was calculated at 0.87 using the KMO index. Further, Bartlett's test of sphericity (6870), which is significant at an error level (0.001), indicates a proper correlation between the items in each factor. The findings of exploratory factor analysis, using the Varimax rotation, revealed five key factors with Eigenvalues more than one remained in the analysis. These factors could explain 71.64 % of the total variance in the variables. The Eigenvalues of factors affecting hospital network management are presented in Table 3.
After exploratory factor analysis, confirmatory factor analysis confirmed the five key factors and 28 components affecting hospital network management, including strategic planning factors (4 components), decision rights factors (6 components), financing factors (6 components), monitoring and evaluation factors (5 components), and accountability factors (7 components), that significant correlation witnessed among them. The most and least factor loadings were assigned to financing and decision rights, with standard coefficients of 0.83 and 0.44, respectively.
In the assessment of components of the strategic planning factor, it was found that the component of the alignment of the hospital network mission with the major policies of the ISSO with standard coefficients of 0.83 had the most influence and component of the formulation of the mission with standard coefficients of 0.74, has the lowest influence at strategic planning. Also, in the decision rights factor, designing and revising the organization chart and purchasing equipment with standard coefficients of 0.84 and 0.74 had the most and least influence, respectively.
The highest and lowest influence components in the financing factor were participation of the Social Security organization in the financing and designing and changing the payment system with standard coefficients of 0.81 and 0.72, respectively. In monitoring and evaluation, the component of monitoring and evaluating of staff performance had the most influence with standard coefficients of 0.82, and the component of monitoring the achievement of goals with standard coefficients of 0.73 had the least influence. The highest and lowest influence components in the accountability factor were the Composition of the board of directors and the presentation of functional and financial reports with standard coefficients of 0.83 and 0.72, respectively. Table 4 demonstrates the standard coefficients of factors and components affecting hospital network management.
Results of research hypotheses testing, regression coefficients, and significance level of structural model are presented in Table 5. As shown, an overview of relationships between variables indicates that all the relationships are confirmed.

Discussion
This study identified the factors influencing the management of hospital networks and explained the role of each factor. The findings demonstrated that the factors of financing with standard coefficients of 0.83 were the most important factor, and decision rights with standard coefficients of 0.44 were the least important factor influencing hospital network management of the ISSO, respectively.In a study by Duran and Salman, factors of institutional arrangements, financing, accountability, and decision rights capacity against responsibility were explained as the main factors of hospital management (4). Also, Nasiripour et al. (10), in a research in 2007, proposed a pattern for corporative hospital management. This pattern included the main factors of decision rights, residual claimant status, market exposure, accountability, and social responsibilities. These findings are consistent with the results of the current research.
According to the results of current research, strategic planning, monitoring the achievement of goals, monitoring and evaluating of employee performance, establishment of quality-of-care committees to oversee the work of physicians, decision rights in construction and repair of buildings, and equipment purchase, are factors affecting the management of hospital network, which warrant our attention. This finding is consistent with Alexander and Schroer's findings in 1985 (20), Dolci et al. (21), Jones et al. (22), and Jackson et al. (23).
The results of the study by Alexander and Schroer in 1985 showed that in the hospital network, most decisions are related to medical staff privileges, adding and removing services at the hospital level, hospital strategic planning, operational and capital budgets, evaluating the hospital CEO's performance, and and appointing the hospital CEO (20). Dolci et al. (21), conducted a study in 2011 to identify the conformity of the objectives of the medical units, the analysis of the efficiency and utilization of resources, the alignment of the mission and values of the organization, the quality and safety standards of the patient, and the degree of coordination between medical units and the health system as a whole. They suggest an evaluation system for specialized hospitals by monitoring performance indicators. Jones et al. (22), in 2017, and Jackson et al. (23), in 2007, also concluded that strategic planning, the systematic development and updating of the` vision, mission, goals, setting of short-term and long-term priorities, and regular evaluation of the functions, are the main factors influencing the management of healthcare organizations.
According to the results of current research, one of the main factors in hospital network management is accountability, which is consistent with the results of the study by Aghazade (6), in 2012 Lewis and Pettersson (24), in 2009 and Lemière et al. (25), in 2012. These researchers believe that the lack of execution of suitable accountability mechanisms in hospitals is one of the major reasons for failure in reforms of hospitals.
The results of this research demonstrated that financing is the most important factor influencing the management of hospital networks. In a study by Kutzin et al. (1), those countries they raised as successful reformers changed away from major health system structural reforms to designing and implementing a coherent and well- functioning health financing system, which is consistent with the results of this study.
According to the current research results, modifying budgeting methods and using operational budgeting methods is one of the important components in hospital network management. This finding is consistent with the findings of researches by Duran and Salman in 2013, La Forgia and Couttolenc in 2008, and Dolci et al. (4, 17, 21) in 2011. Further, the findings of this study showed that the hospital's responsibility against the probable deficiencies can be effective in hospital management, which is consistent with the results of the study by Nasiripour et al. (10), in 2007 and Lemière et al. (25), in 2012.
The findings of the present study demonstrated that decision rights in staff recruitment and dismiss, are one of the main factors in the improvement of hospital network management. Based on the research by De Geyndt in 2017 and La Forgia and Couttolenc in 2008, decision rights to staff recruitment, dismissal, promotion, and transfer can lead to an improvement in the hospitals' performance (8, 17), which is consistent with the results of the present study. In this regard, the findings of a research by Pettersen et al. (7) in 2012 indicated that extensive area for decision making in staff recruitment and dismissal might raise problems such as ambiguity and opportunism for the boards, which is inconsistent with this research.
This research had some limitations. Inclusion criteria were used for the interviewees, so some experts may have been left out. If the participants had changed, our findings would have been different. However, the strength of this study was its global design and including ISSO hospitals across the country.
Conclusion
This study specified factors affecting the management of hospital networks. Considering the exigency to modify and improve the management of ISSO's hospitals and based on the present study, it seems that policymakers and managers of social security organization hospitals should pay more attention to human resources management, financing, using operational budgeting methods, payment systems, property management, monitoring, and evaluation systems, using suitable accountability mechanism and accent on customer satisfaction in developing a strategic plan. The findings of the current research can be used to manage public and private hospitals and other healthcare organizations.
Acknowledgments
The authors would like to thank the ISSO experts for their assistance in the data collection process.
Conflict of interests
The authors declared no conflict of interests.
Authors' contributions
Mohammadi F, Masoudi Asl I, Mahfoozpour S and Hessam S designed research; Masoudi Asl I, Mahfoozpour S and Mohammadi F conducted research; Hessam S analyzed data; and Mohammadi F, Masoudi Asl I and Mahfoozpour S wrote the paper. Masoudi Asl I had primary responsibility for final content. All authors read and approved the final manuscript.
Funding
It was not financially supported.
Type of Study: Original article |
Subject:
Healt care Management
Received: 2021/02/3 | Accepted: 2021/10/4 | Published: 2021/10/4
Received: 2021/02/3 | Accepted: 2021/10/4 | Published: 2021/10/4
References
1. Kutzin J, Jakab M, Cashin C. Lessons from health financing reform in central and Eastern Europe and the former Soviet :union:. Health Economics, Policy and Law. 2010; 1-13. [DOI:10.1017/S1744133110000010]
2. Nazari M, Riahi L, Tabibi SJ, Mahmoudi Majdabadi Farahani M. Design of the pattern of effective environmental factors for outsourcing the services in public hospitals. Alborz Univ Med J (AUMJ). 2018; 7(4): 333-44. doi: 10.29252/aums.7.4.333. [DOI:10.29252/aums.7.4.333]
3. Rahbar A, HamidiParsa H, Khosravi M. The assessing performance of educational therapeutic hospitals dependent to qom and kashan medical sciences and health services universities and their comparison using by the pabon lasso model. Health Inf Manage. 2014; 11(3): 370.
4. Duran A, Saltman RB. Innovative strategies in governing public hospitals. Euro health. 2013; 19(1): 3-7.
5. Yang YH. Research on China's public hospital management: From perspective of implementation issues. Chinese Medical Journal. 2016; 129(3): 357. [DOI:10.4103/0366-6999.174505]
6. Aghazadeh S, Aliyev AQ, Ebrahimnazhad M. Overview of the management reform of the health institutions. Journal of Basic and Applied Scientific Research. 2012; 2(3): 3036-45.
7. Pettersen IJ, Nyland K, Kaarboe K. Governance and the functions of boards: An empirical study of hospital boards in Norway. Health Policy. 2012; 107(2-3): 269-75. [DOI:10.1016/j.healthpol.2012.07.006]
8. De Geyndt W. Does autonomy for public hospitals in developing countries increase performance? Evidence-based case studies. Social Science & Medicine (1982). 2017; 179:74-80. [DOI:10.1016/j.socscimed.2017.02.038]
9. Mirzaei S, Noorihekmat S, Oroomiei N, Vali L. Administrative challenges of clinical governance in military and university hospitals of Kerman/Iran. The International Journal of Health Planning and Management. 2019; 34(2): 1293-301. [DOI:10.1002/hpm.2774]
10. Nasiripour AA, Ali Mohammadzadeh KH, Ardan Sh, Raeeisi P. Design the privatization pattern for Administration of the Social Security hospitals. Journal of Food Sciences and Nutrition. 2007; 5(1): 73-83.
11. Erwin CO, Landry AY, Livingston AC, Dias A. Effective governance and hospital boards revisited: Reflections on 25 years of research. Med Care Res Rev. 2018; 76(2): 131-66. [DOI:10.1177/1077558718754898]
12. London JD. The promises and perils of hospital autonomy: Reform by decree in Vietnam. Soc Sci Med. 2013; 96: 232-40. [DOI:10.1016/j.socscimed.2013.07.009]
13. Bravi F, Gibertoni D, Marcon A, Sicotte C, Minvielle E, Rucci P, et al. Hospital network performance: A survey of hospital stakeholders' perspectives. Health Policy. 2013; 109(2): 150-7. [DOI:10.1016/j.healthpol.2012.11.003]
14. American Hospital Association. Fast facts on U.S. hospitals, 2019. Available from URL: https://www.healthycommunities.org/statistics/2020-01-07-archived-fast-facts-us-hospitals-2019.
15. Toro TM, Cueto E, Giuffrida A, Arango C, López A. "Public Hospitals and Health Care Reform in Colombia." Bogotá. Forthcoming, Lancet. 2007.
16. Fidler AH, Haslinger RR, Hofmarcher MM, Jesse M, Palu T. Incorporation of public hospitals: A "silver bullet" against overcapacity, managerial bottlenecks and resource constraints?: Case studies from Austria and Estonia. Health Policy. 2007; 81(2-3): 328-38. [DOI:10.1016/j.healthpol.2006.06.007]
17. LaForgia GM, Couttolenc BF. Hospital performance in Brazil: The search for excellence. Washington, DC: The World Bank publication. 2008. [DOI:10.1596/978-0-8213-7358-3]
18. Department of Treatment. A look at the programs and activities of the Social Security Organization in 2017. Tehran: The Iranian Social Security Organization; 2018. Report NO: EC-45. [In Persian]
19. Barati O, Sadeghi A, Khammarnia M, Siavashi E. Investigation of hospitals management challenges: A qualitative study in Shiraz hospitals. Sadra Medical Sciences Journal. 2017; 4(3): 149-160. [In Persian]
20. Alexander JA, Schroer KA. Governance in multihospital systems: An assessment of decision-making responsibility. Hospital & Health Services Administration. 1985; 30(2): 9-20.
21. Dolci GF, Gas HG, Galván HR. Monitoring evaluation system for high-specialty hospitals. Gac Med Mex. 2011; 147(5): 411-9.
22. Jones L, Pomeroy L, Robert G, Burnett S, Anderson JE, Fulop NJ. How do hospital boards govern for quality improvement? A mixed methods study of 15 organizations in England. BMJ Qual Saf. 2017; 26(12): 978-86.
23. jackson S, Perkins F, Khandor E, Cordwell L, Homann S, Buasai S. Integrated health promotion strategies: A contribution to tackling current and future health challenges. Oxford University Journal. 2007; (2): 75-83. [DOI:10.1093/heapro/dal054]
24. Lewis M, Pettersson G. Management in health care delivery: Raising performance. The World Bank. 2009. [DOI:10.1596/1813-9450-5074]
25. Lemière, C, Turbat V, Puret, J. A tale of excessive hospital autonomy: An evaluation of the hospital reform in senegal. The World Bank. 2012.
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |