Volume 6, Issue 2 (5-2022)
EBHPME 2022, 6(2): 100-109 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Mokhtari A, Nabilou B, Aghlmand S, Yusefzadeh H. Productivity Analysis of Medical Record Department in Hospitals Affiliated with Urmia University of Medical Sciences. EBHPME 2022; 6 (2) :100-109
URL: http://jebhpme.ssu.ac.ir/article-1-386-en.html
URL: http://jebhpme.ssu.ac.ir/article-1-386-en.html
Department of Health Economics and Management, School of Public Health, Urmia University of Medical Sciences, Urmia, Iran , yusefzadeh.h@umsu.ac.ir
Full-Text [PDF 578 kb]
(565 Downloads)
| Abstract (HTML) (2151 Views)
Full-Text: (448 Views)
Background: The importance of paying attention to improving productivity in different health system departments has become increasingly evident. This is due to increased costs of health care goods and services, limited resources and production facilities. This study aims to measure the productivity of hospitals' Medical Records Departments (MRD) affiliated with Urmia University of Medical Sciences to provide a comprehensive analysis of their performance.
Methods: In this study, total productivity and total factor productivity changes of medical record departments in hospitals affiliated with Urmia University of Medical Sciences were calculated. This was conducted through Kendrick-Creamer and Malmquist indexes in 2016-2020, and has examined the trend of each one of them. Input variables included the number of personnel and equipment. Output variables encompassed the number of outpatient and inpatient medical records prepared for patients, responses to letters, and patients referred to the studied MRD. After estimating the production function, the elasticity of production factors and the return to the scale of medical record departments were calculated.Total productivity changes and production function were estimated via Deap2,1 and Frontier4,1 softwares by applying input minimization and variable returns to scale assumptions.
Results: The results of the Malmquist index indicated that the average total productivity changes of medical records departments of hospitals during the study period were equal to 1,096. This is greater than one; therefore, it can be concluded that productivity has decreased by about 9.600 % during the study period. Changes in technological efficiency have had the greatest impact on reducing productivity, to other factors. In addition, the results of Kendrick-Creamer index during the years under review demonstrated that the average total productivity of production factors obtained, was equal to 18725.530 services.
Conclusion: There is decreased productivity due to technological changes in the studied departments. This is because of the lack of sufficient knowledge of the medical records department staff in the use of technology and equipment for providing efficient services . Holding training courses for the appropriate use of technology by personnel can be useful in this regard.
Key words: Medical record department, Efficiency, Productivity, Urmia
Calculating productivity enables MRD managers to monitor the trend of productivity changes, identify potential problems, and take timely corrective action. Therefore, measuring total factor productivity (TFP) changes, a criterion for describing the correct and optimal use of production factors, and identifying the factors affecting these changes will lead to adopting corrective measures to improve productivity (12).
data envelopment analysis (DEA) and Kendrick-Creamer index are the most important and accurate methods of measuring productivity. Kendrick-Creamer index measures the total and final productivity of production factors in hospital's MRD. Total Factor Productivity (TFP) is defined as the ratio of total production to the sum of all inputs consumed. In contrast, final productivity is the amount of change in total production per unit of change in the use of the production factor. The amount of changes in total productivity for all MRDs of hospitals can be calculated using the DEA method by the Malmquist index. It is an accurate measure of productivity monitoring (13). In addition, it divides productivity changes into changes resulting from technological, managerial, and scale efficiency (14-16).
There is no study conducted to evaluate the productivity of MRD in Iranian hospitals, especially using the Kendrick Creamer index. The results reported by Dargahi et al. (10), Nabilou et al. (16), Li et al. (13), Silwal et al. (17), and Moffat et al. (18) confirmed to the productivity in hospitals.
This study aims to determine the total factor productivity changes. Furthermore, it measures the productivity of production factors in the MRD of hospitals affiliated with Urmia University of Medical Sciences during 2016-2020. It is conducted in order to plan for improving the performance of MRD as well as the allocation of resources to this vital department optimally.
Materials and Methods
This was a descriptive-analytical study. It examined all MRDs of general medical and teaching hospitals affiliated with Urmia University of Medical Sciences, West Azerbaijan (including 24 hospitals) ,2016-2020. The results MRD of each hospital with the number assigned will be provided to that hospital to comply with ethical considerations. The required data and information were collected from the studied hospitals and the vice-chancellor for treatment affairs of Urmia University of Medical Sciences. It was conducted using checklists designed by the researcher.
According to the results of previous studies, the authors selected a combination of the most important and common inputs and outputs to estimate total factor productivity changes. These data included: The number of outpatient and inpatient medical records prepared for patients in the MRD, the number of responses to letters and patients referred to the department as output, variables about the number of personnel working in the MRD, holders of associate and lower and bachelor's and higher degrees as well as the number of equipment (computer, printer, wristband printer, barcode reader and ICD-10 {International Classification of Diseases) books} were considered as inputs (10,19,20).
At first, productivity changes of the studied hospitals were evaluated for the years 2016-2020 using the non-parametric method of DEA and Malmquist index through Deap2.1 software. This was done after the required data were collected from the MRDs of the hospitals affiliated with Urmia University of Medical Sciences.
The Malmquist productivity index is defined using distance functions as follows:
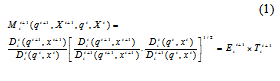
In this formula, (total factor productivity index) is equal to multiplying technological changes
(total factor productivity index) is equal to multiplying technological changes , [which is measured by transferring the frontier production function between period t+1 and t] by efficiency changes (
, [which is measured by transferring the frontier production function between period t+1 and t] by efficiency changes ( ) in the same period.
) in the same period.  is the input distance function,
is the input distance function,  is the output and input values in the period t+1, and
is the output and input values in the period t+1, and  is equal to the output and input values in period t, respectively (18). Finally, the total productivity changes for the MRD of each hospital are obtained from the following equation:
is equal to the output and input values in period t, respectively (18). Finally, the total productivity changes for the MRD of each hospital are obtained from the following equation:
Total productivity changes = managerial efficiency changes × scale efficiency changes × Technological changes
If the Malmquist index is less than one based on minimizing production factors, it means that performance improves, while a value greater than one indicates performance reduction over time (17).
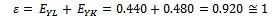
Then, the Kendrick-Creamer index was used to measure the total productivity of production factors. The existence of total production elasticity relative to the production factors is necessary to calculate the mentioned index. It requires estimating the production function to measure these elasticities. The parametric method of Stochastic Frontier Analysis (SFA) and Frontier4,1 software were used to estimate the function. In the following Cobb-Douglas function, the power of each of the production factors indicates its corresponding elasticity:
 (2)
(2)
At this stage, the total productivity of the hospitals under the study's production factors was calculated using the Kendrick-Creamer index and the elasticity of production factors. The mathematical form of the Kendrick-Creamer function is as follows:
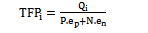 (3)
(3)
Where is total productivity of MRD,
is total productivity of MRD,  output. The number of outpatient and inpatient medical records for patients in the MRD and the number of responses to letters and clients referred to this department were used as output in this study.
output. The number of outpatient and inpatient medical records for patients in the MRD and the number of responses to letters and clients referred to this department were used as output in this study.  number of personnel input, N is the number of equipment input,
number of personnel input, N is the number of equipment input,  the elasticity of personnel input and
the elasticity of personnel input and e n
This article was a part of master's thesis (ethics code: IR.UMSU.REC.1398.350) that Urmia University of Medical Sciences supported.
Results
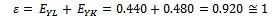
Kendrick-Creamer index was used to calculate the total factor productivity. The existence of total production elasticity relative to production factors of personnel and capital was necessary to calculate the mentioned index, which required estimating the production function to calculate these factors. Frontier4,1 software was used to estimate the production function. The results of estimating the production function were as follows:
LnY = 10.110 + 0.440 LnL + 0.480 LnK
Standard deviation (0.140) (0.190) (0.250)
t statistics (71.040) (2.320) (1.900)
LR = 13.400
As can be seen, all coefficients are statistically and significantly different from 0. Given that the obtained LR was above 4, the estimated function was suitable.
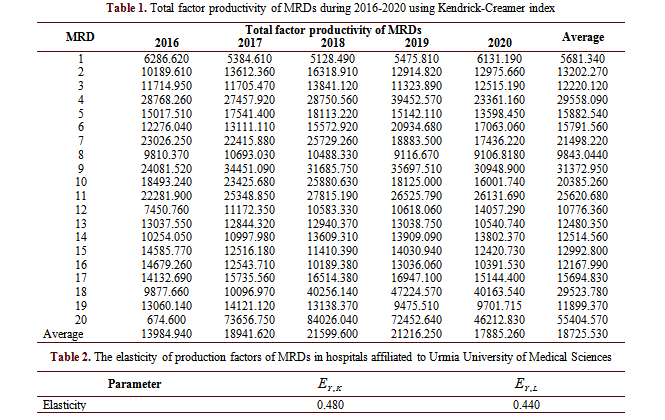
In the next step, the total factor productivity of MRD in hospitals affiliated with Urmia University of Medical Sciences was calculated using the elasticity of the production factors. According to Table 1, the average total productivity reached 17885.260 in 2020 from 13984.940 in 2016 during a fluctuation. That is, the total MRDs of university hospitals, on average, for each unit of labor (personnel) and capital (equipment available in the MRD) have been able to create 17885.260 outputs (services provided in the MRD) in 2020.
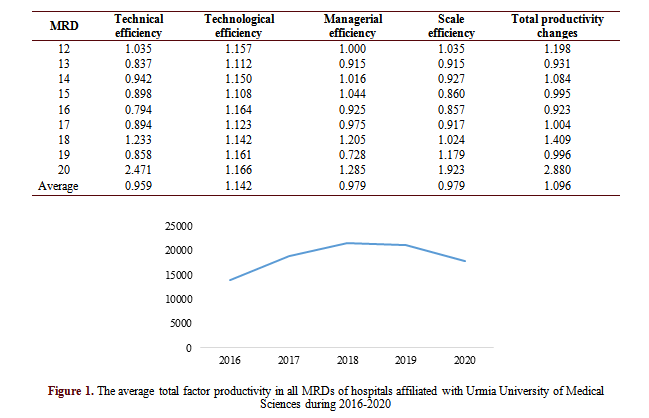
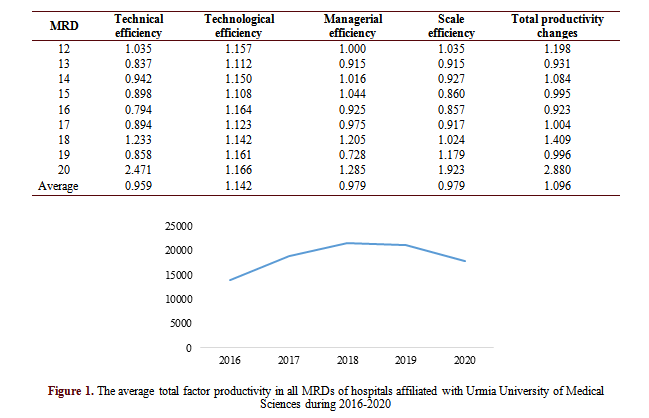
Figure 1 shows the trend of the average total productivity of production factors in all MRDs of hospitals affiliated with Urmia University of Medical Sciences during the years 2016-2020.
The sum of elasticities of the production factors (function coefficient) indicated the return to scale.
The elasticities of the production factors in the Cobb-Douglas production function with logs on both sides have the same function coefficient. The elasticity of each of the production factors is shown in the Table 2.
The function coefficient obtained was approximately equal to one by summing the elasticities, which represents constant return to the scale.
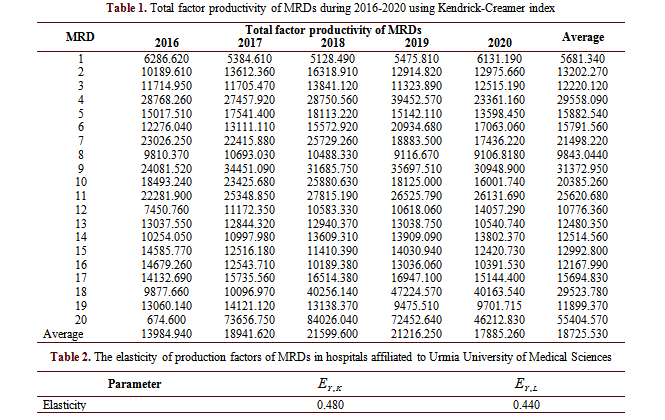
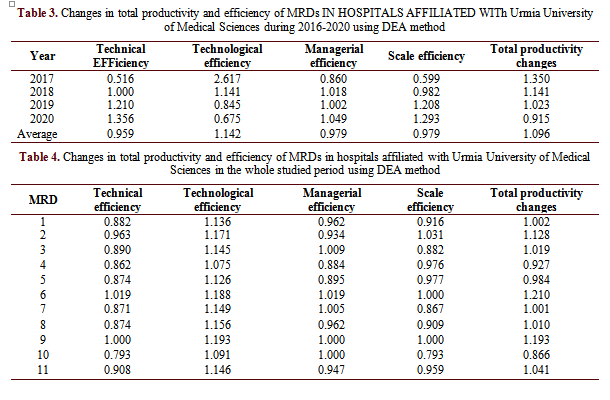
The results of calculating total factor productivity changes, using Deap2,1 software and analysis of its changes based on the factors affecting it, are shown in Table 3.
As the calculations in the above table suggest, during the period under study, the average total productivity change was equal to 1.096. Given that the number obtained was greater than one, productivity decreased during this period. Also, the average technological efficiency change was 1.142, the average technical efficiency change, 0.959, the average managerial efficiency change, 0.979, and the average scale efficiency change was 0.979. During the studied period, technical, managerial, and scale efficiency positively affected productivity, while it was observed that technological efficiency had a negative effect on productivity.
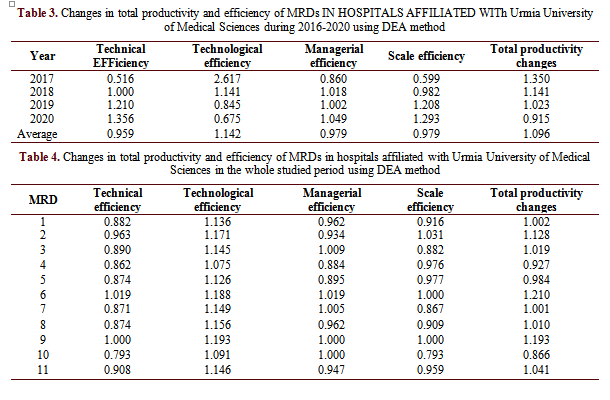
The results of the Table 4 show that hospitals 20 (2.880) and 10 (0.866) had the worst and best performance among the MRDs of the studied hospitals, respectively. Moreover, the departments 10 (0.793), 4 (1.075), 19 (0.728), and 10 (0.793) demonstrated the highest improvement in the index of changes in technical efficiency, technological efficiency, managerial efficiency, and scale efficiency during the years 2016-2020 respectively. Total productivity changes of MRDs of hospitals affiliated with Urmia University of Medical Sciences were largely affected by the negative effect of technological efficiency changes. As a result, it is necessary to pay attention to how to use new technologies to increase productivity.
Discussion
The use of physical, technical, and human resources optimally is the main motivation to use scientific and applied methods to evaluate the activities and performance of organizations. One of the most important performance appraisal indicators for combining factors and production resources to achieve the goal of optimal resource allocation and cost reduction is productivity. The present study aims to investigate the productivity of MRD in hospitals affiliated with Urmia University of Medical Sciences.
Kendrick-Creamer index was used to calculate the average total production factor productivity of MRDs of the studied hospitals in all the studied years, equal to 18725.530 . In other words, all MRDs of the hospitals under study have provided services equal to 18725.530, on average, for each unit of total production factors. This index revealed that productivity has increased in all studied years except 2019.
Kendrick-Creamer index was used to calculate the average total production factor productivity of MRDs of the studied hospitals in all the studied years, which was equal to 18725.530. In other words, all MRDs of the hospitals under study have been able to provide services equal to 18725.530, on average, for each unit of total production factors. The results of this index indicated that productivity increased in all the years except for 2019.
In this study, the average total productivity changes of MRDs in hospitals affiliated with Urmia University of Medical Sciences, using the Malmquist index, was equal to 1.096. The number obtained is greater than one. This means the total production factor productivity of MRDs of the studied hospitals has decreased despite the increasing trend of productivity growth during the years 2016-2020. Furthermore, the amount of this decrease has been 9.600 %. In the meantime, technological efficiency changes have had the greatest impact on reducing productivity compared to other factors. In other words, the MRDs under study did not appropriately benefit from technological advances. Therefore, we need to look at how new technologies can be used to increase productivity. According to the results reported by Sahin et al. (21), due to technological advances in providing services followed by government investment, the total productivity of Turkish hospitals has increased in public hospitals of that country (21). Thus, improving technology can play an important role in increasing the productivity of MRDs, especially in large hospitals. During the studied period, technical, managerial, and scale efficiency of MRDs in hospitals also positively affected productivity.
In this study, the sum of elasticities of production factors (function coefficient) was approximately equal to one. The return to scale was almost constant in the MRDs of the studied hospitals. This means that a one percent change in the amount of utilization of production factors leads to a one percent change in the amount of production.
The results of the Malmquist index indicated that the average technical efficiency of MRDs of hospitals was 0.959; that is, these hospitals can increase their output by 4.100 % without increasing the amount of production inputs and because of the optimal use of resources.
The average managerial efficiency has been obtained at 0.979 in this study. In other words, productivity can be increased up to 2.100 % .It can be conducted using the correct management techniques and motivation of the staff in MRDs of the hospitals without changing the amount of inputs. Therefore, effective steps can be taken to improve the productivity of MRDs in these hospitals by proper management, using the opinions of staff, and creating favorable working environments.
The average scale efficiency was 0.979 in this study. This means that an annual average of 2.100 % can be added to the output of MRDs in the studied hospitals. This is because of the savings caused by providing services on a large scale. Therefore, departments with increasing returns to scale should increase the level of providing services due to economic justification. Moreover, departments with decreasing returns to scale should review the overall structure of their department and adjust their capital and additional personnel inputs to avoid negative marginal production.
The main reason for decreased total factor productivity can be the lack of sufficient knowledge of the personnel in utilizing the existing equipment and technologies of this department for providing services in the right way. Therefore, training courses should be provided for the correct use of the equipment by personnel in departments, where the main reason for the decreased productivity is technological changes. In this study, the average annual output of MRDs has been reduced by 14.200 % due to technological changes. According to the results of Malmquist index, the range of changes in total factor productivity of MRDs of the studied hospitals in the review period was between 0.866 and 2.880. Therefore, productivity has increased only in 7 departments out of 20 and has decreased in another 13 departments. Therefore, high efficiency departments can be considered a model for other departments in terms of using production factors to increase efficiency and productivity.
In this regard, effective measures such as quantitative and qualitative improvement of providing services, continuous performance appraisal, and the optimal use of personnel and equipment of departments to increase the efficiency of hospital MRDs were proposed. Moreover, by continuously monitoring the performance of MRDs, the results can be used for planning and policy-making and avoiding wasting resources. The causes of their progress or decline can be determined by examining trends in total productivity changes. According to the results of the indexes calculated in this study, the authors can identify the amount of total productivity changes and its trend in MRDs of hospitals. Therefore, it is suggested that managers pay special attention to these methods to improve their productivity and performance.
Most of the studies on the productivity of total factor production in the health system have focused on the medical departments. So far, only one domestic study has been conducted on the productivity of MRDs at Tehran University of Medical Sciences through the Malmquist index. There have been no studies for the researchers to compare them with the results of this study. Therefore, the main limitation of this study was the impossibility of comparing the results of the present study with other studies. This research is the only study investigating the total factor productivity of all MRDs. It used two indexes of Malmquist and Kendrick-Creamer, which is considered its most significant strength compared to the study conducted by Dargahi et al. (10) They investigated changes in the productivity of the MRDs of Tehran University of Medical Sciences hospitals through the years 2006-2007. Assuming maximization of the production factors, they used the DEA method (Malmquist index), and calculated total productivity changes in their study. It was equal to 0.938. This number indicates that the productivity of MRDs in hospitals has decreased during the studied period due to the wrong assumption adopted to calculate the amount of productivity changes. Moreover, technological and technical efficiency changes had the highest effect on reducing the amount of total productivity changes. Changes in managerial efficiency and scale efficiency were in the next ranks, respectively (10). This was consistent with the results of this study. In general, the health system cannot control the number of patients referred to hospitals; thus, it is wrong to use the assumption of output maximization in calculations. Nouraei Motlagh et al. (19), in a study, investigated changes in the total factor productivity in hospitals affiliated with Lorestan University of Medical Sciences in 2010-2016. They used the DEA method for this purpose. In this study, the average total productivity change of hospitals during the studied period was 1.023. This indicates that productivity has decreased during the studied period, and technological changes had the maximum negative effect on productivity reduction compared to other factors (19). This is consistent with the results of this study. Furthermore, technological changes in the studies by Torabipour in Ahvaz hospitals (22), Krigia in Angola hospitals (23), and Yawe in Uganda hospitals (24) were the main cause of decreased total productivity, which is consistent with the results of the present study. Productivity of all departments in the hospital can be increased by upgrading technology and using the up-to-date equipment.
Conclusion
In this study, insufficient knowledge of personnel's MRD in the correct use of technology for providing services was the leading cause of decreased productivity. Therefore, providing instructions for correct use of technology can be helpful for personnel. The results of the Kendrick-Creamer and Malmquist indices can help managers improve productivity, and thus, reduce the costs of hospitals' medical records departments.
Acknowledgements
The authors would like to thank MRDs’ managers for their collaboration in data gathering.
Conflict of interests
Authors declared no conflict of interests.
Authors' contributions
Mokhtari A and Yusefzadeh H designed research; Mokhtari A, Nabilou B, Aghlmand S and Yusefzadeh H conducted research; Yusefzadeh H analyzed data; and Nabilou B and Mokhtari A wrote the paper. Yusefzadeh H had primary responsibility for final content. All authors read and approved the final manuscript.
Funding
This study was supported by Urmia University of Medical Sciences.
Methods: In this study, total productivity and total factor productivity changes of medical record departments in hospitals affiliated with Urmia University of Medical Sciences were calculated. This was conducted through Kendrick-Creamer and Malmquist indexes in 2016-2020, and has examined the trend of each one of them. Input variables included the number of personnel and equipment. Output variables encompassed the number of outpatient and inpatient medical records prepared for patients, responses to letters, and patients referred to the studied MRD. After estimating the production function, the elasticity of production factors and the return to the scale of medical record departments were calculated.Total productivity changes and production function were estimated via Deap2,1 and Frontier4,1 softwares by applying input minimization and variable returns to scale assumptions.
Results: The results of the Malmquist index indicated that the average total productivity changes of medical records departments of hospitals during the study period were equal to 1,096. This is greater than one; therefore, it can be concluded that productivity has decreased by about 9.600 % during the study period. Changes in technological efficiency have had the greatest impact on reducing productivity, to other factors. In addition, the results of Kendrick-Creamer index during the years under review demonstrated that the average total productivity of production factors obtained, was equal to 18725.530 services.
Conclusion: There is decreased productivity due to technological changes in the studied departments. This is because of the lack of sufficient knowledge of the medical records department staff in the use of technology and equipment for providing efficient services . Holding training courses for the appropriate use of technology by personnel can be useful in this regard.
Key words: Medical record department, Efficiency, Productivity, Urmia
Introduction
Healthcare sector is considered one of the most important service centers. Its performance is one of the indicators of development and social welfare. Its economic analysis, accordingly, is vital for health decision-makers (1-3). Hospital is one of the most critical and influential segments of society in all health systems which plays an essential role in providing medical services and health promotion (4, 5). Thus, hospitals benefit from a large number of trained and specialized personnel in the health care system in many countries and consume about 50 to 80 percent of health funding (6). National statistics in Iran revealed that about 40 % of government health expenditures are related to hospitals (7, 8). Thus, health policymakers and decision-makers should always consider managing hospitals and their departments favorably as the most important center for providing health services. Medical Record Department (MRD) is one of these hospital departments. There, all medical service documents provided to a patient in the hospital are kept in order of date. They are used for subsequent treatment of patients, research and training, and the review of provided services in terms of quantity and quality. MRD is considered the most important and richest source of information for evaluating and planning healthcare services in health organizations such as hospitals. In this department, the patient's medical record is the most essential tool for storing and retrieving information, analyzing health care. It also provides all the information related to the patient's medical history, diseases, health risks, diagnoses, tests, examinations, treatment methods, disease course, and the patient's response to treatment and follow-up (9).
Waste of resources is one of the consequences of poor management of hospitals' MRD. Available resources can be used to provide more services and improve service quality by preventing and reducing resource waste (10). Therefore, improving productivity has the most effect on cost control planning and prevention of waste of resources in different departments of hospitals (11). MRDs are no exception. It is necessary to implement effective strategies by managers of these departments to reduce costs and increase productivity. Calculating productivity enables MRD managers to monitor the trend of productivity changes, identify potential problems, and take timely corrective action. Therefore, measuring total factor productivity (TFP) changes, a criterion for describing the correct and optimal use of production factors, and identifying the factors affecting these changes will lead to adopting corrective measures to improve productivity (12).
data envelopment analysis (DEA) and Kendrick-Creamer index are the most important and accurate methods of measuring productivity. Kendrick-Creamer index measures the total and final productivity of production factors in hospital's MRD. Total Factor Productivity (TFP) is defined as the ratio of total production to the sum of all inputs consumed. In contrast, final productivity is the amount of change in total production per unit of change in the use of the production factor. The amount of changes in total productivity for all MRDs of hospitals can be calculated using the DEA method by the Malmquist index. It is an accurate measure of productivity monitoring (13). In addition, it divides productivity changes into changes resulting from technological, managerial, and scale efficiency (14-16).
There is no study conducted to evaluate the productivity of MRD in Iranian hospitals, especially using the Kendrick Creamer index. The results reported by Dargahi et al. (10), Nabilou et al. (16), Li et al. (13), Silwal et al. (17), and Moffat et al. (18) confirmed to the productivity in hospitals.
This study aims to determine the total factor productivity changes. Furthermore, it measures the productivity of production factors in the MRD of hospitals affiliated with Urmia University of Medical Sciences during 2016-2020. It is conducted in order to plan for improving the performance of MRD as well as the allocation of resources to this vital department optimally.
Materials and Methods
This was a descriptive-analytical study. It examined all MRDs of general medical and teaching hospitals affiliated with Urmia University of Medical Sciences, West Azerbaijan (including 24 hospitals) ,2016-2020. The results MRD of each hospital with the number assigned will be provided to that hospital to comply with ethical considerations. The required data and information were collected from the studied hospitals and the vice-chancellor for treatment affairs of Urmia University of Medical Sciences. It was conducted using checklists designed by the researcher.
According to the results of previous studies, the authors selected a combination of the most important and common inputs and outputs to estimate total factor productivity changes. These data included: The number of outpatient and inpatient medical records prepared for patients in the MRD, the number of responses to letters and patients referred to the department as output, variables about the number of personnel working in the MRD, holders of associate and lower and bachelor's and higher degrees as well as the number of equipment (computer, printer, wristband printer, barcode reader and ICD-10 {International Classification of Diseases) books} were considered as inputs (10,19,20).
At first, productivity changes of the studied hospitals were evaluated for the years 2016-2020 using the non-parametric method of DEA and Malmquist index through Deap2.1 software. This was done after the required data were collected from the MRDs of the hospitals affiliated with Urmia University of Medical Sciences.
The Malmquist productivity index is defined using distance functions as follows:
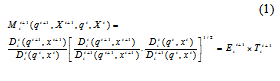
In this formula,
 (total factor productivity index) is equal to multiplying technological changes
(total factor productivity index) is equal to multiplying technological changes , [which is measured by transferring the frontier production function between period t+1 and t] by efficiency changes (
, [which is measured by transferring the frontier production function between period t+1 and t] by efficiency changes ( ) in the same period.
) in the same period.  is the input distance function,
is the input distance function,  is the output and input values in the period t+1, and
is the output and input values in the period t+1, and  is equal to the output and input values in period t, respectively (18). Finally, the total productivity changes for the MRD of each hospital are obtained from the following equation:
is equal to the output and input values in period t, respectively (18). Finally, the total productivity changes for the MRD of each hospital are obtained from the following equation:Total productivity changes = managerial efficiency changes × scale efficiency changes × Technological changes
If the Malmquist index is less than one based on minimizing production factors, it means that performance improves, while a value greater than one indicates performance reduction over time (17).
Then, the Kendrick-Creamer index was used to measure the total productivity of production factors. The existence of total production elasticity relative to the production factors is necessary to calculate the mentioned index. It requires estimating the production function to measure these elasticities. The parametric method of Stochastic Frontier Analysis (SFA) and Frontier4,1 software were used to estimate the function. In the following Cobb-Douglas function, the power of each of the production factors indicates its corresponding elasticity:
 (2)
(2)At this stage, the total productivity of the hospitals under the study's production factors was calculated using the Kendrick-Creamer index and the elasticity of production factors. The mathematical form of the Kendrick-Creamer function is as follows:
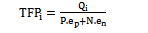 (3)
(3)Where
 is total productivity of MRD,
is total productivity of MRD,  output. The number of outpatient and inpatient medical records for patients in the MRD and the number of responses to letters and clients referred to this department were used as output in this study.
output. The number of outpatient and inpatient medical records for patients in the MRD and the number of responses to letters and clients referred to this department were used as output in this study.  number of personnel input, N is the number of equipment input,
number of personnel input, N is the number of equipment input,  the elasticity of personnel input and
the elasticity of personnel input and This article was a part of master's thesis (ethics code: IR.UMSU.REC.1398.350) that Urmia University of Medical Sciences supported.
Results
Kendrick-Creamer index was used to calculate the total factor productivity. The existence of total production elasticity relative to production factors of personnel and capital was necessary to calculate the mentioned index, which required estimating the production function to calculate these factors. Frontier4,1 software was used to estimate the production function. The results of estimating the production function were as follows:
LnY = 10.110 + 0.440 LnL + 0.480 LnK
Standard deviation (0.140) (0.190) (0.250)
t statistics (71.040) (2.320) (1.900)
LR = 13.400
As can be seen, all coefficients are statistically and significantly different from 0. Given that the obtained LR was above 4, the estimated function was suitable.
In the next step, the total factor productivity of MRD in hospitals affiliated with Urmia University of Medical Sciences was calculated using the elasticity of the production factors. According to Table 1, the average total productivity reached 17885.260 in 2020 from 13984.940 in 2016 during a fluctuation. That is, the total MRDs of university hospitals, on average, for each unit of labor (personnel) and capital (equipment available in the MRD) have been able to create 17885.260 outputs (services provided in the MRD) in 2020.
Figure 1 shows the trend of the average total productivity of production factors in all MRDs of hospitals affiliated with Urmia University of Medical Sciences during the years 2016-2020.
The sum of elasticities of the production factors (function coefficient) indicated the return to scale.
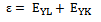
The elasticities of the production factors in the Cobb-Douglas production function with logs on both sides have the same function coefficient. The elasticity of each of the production factors is shown in the Table 2.
The function coefficient obtained was approximately equal to one by summing the elasticities, which represents constant return to the scale.
The results of calculating total factor productivity changes, using Deap2,1 software and analysis of its changes based on the factors affecting it, are shown in Table 3.
As the calculations in the above table suggest, during the period under study, the average total productivity change was equal to 1.096. Given that the number obtained was greater than one, productivity decreased during this period. Also, the average technological efficiency change was 1.142, the average technical efficiency change, 0.959, the average managerial efficiency change, 0.979, and the average scale efficiency change was 0.979. During the studied period, technical, managerial, and scale efficiency positively affected productivity, while it was observed that technological efficiency had a negative effect on productivity.
The results of the Table 4 show that hospitals 20 (2.880) and 10 (0.866) had the worst and best performance among the MRDs of the studied hospitals, respectively. Moreover, the departments 10 (0.793), 4 (1.075), 19 (0.728), and 10 (0.793) demonstrated the highest improvement in the index of changes in technical efficiency, technological efficiency, managerial efficiency, and scale efficiency during the years 2016-2020 respectively. Total productivity changes of MRDs of hospitals affiliated with Urmia University of Medical Sciences were largely affected by the negative effect of technological efficiency changes. As a result, it is necessary to pay attention to how to use new technologies to increase productivity.
Discussion
The use of physical, technical, and human resources optimally is the main motivation to use scientific and applied methods to evaluate the activities and performance of organizations. One of the most important performance appraisal indicators for combining factors and production resources to achieve the goal of optimal resource allocation and cost reduction is productivity. The present study aims to investigate the productivity of MRD in hospitals affiliated with Urmia University of Medical Sciences.
Kendrick-Creamer index was used to calculate the average total production factor productivity of MRDs of the studied hospitals in all the studied years, equal to 18725.530 . In other words, all MRDs of the hospitals under study have provided services equal to 18725.530, on average, for each unit of total production factors. This index revealed that productivity has increased in all studied years except 2019.
Kendrick-Creamer index was used to calculate the average total production factor productivity of MRDs of the studied hospitals in all the studied years, which was equal to 18725.530. In other words, all MRDs of the hospitals under study have been able to provide services equal to 18725.530, on average, for each unit of total production factors. The results of this index indicated that productivity increased in all the years except for 2019.
In this study, the average total productivity changes of MRDs in hospitals affiliated with Urmia University of Medical Sciences, using the Malmquist index, was equal to 1.096. The number obtained is greater than one. This means the total production factor productivity of MRDs of the studied hospitals has decreased despite the increasing trend of productivity growth during the years 2016-2020. Furthermore, the amount of this decrease has been 9.600 %. In the meantime, technological efficiency changes have had the greatest impact on reducing productivity compared to other factors. In other words, the MRDs under study did not appropriately benefit from technological advances. Therefore, we need to look at how new technologies can be used to increase productivity. According to the results reported by Sahin et al. (21), due to technological advances in providing services followed by government investment, the total productivity of Turkish hospitals has increased in public hospitals of that country (21). Thus, improving technology can play an important role in increasing the productivity of MRDs, especially in large hospitals. During the studied period, technical, managerial, and scale efficiency of MRDs in hospitals also positively affected productivity.
In this study, the sum of elasticities of production factors (function coefficient) was approximately equal to one. The return to scale was almost constant in the MRDs of the studied hospitals. This means that a one percent change in the amount of utilization of production factors leads to a one percent change in the amount of production.
The results of the Malmquist index indicated that the average technical efficiency of MRDs of hospitals was 0.959; that is, these hospitals can increase their output by 4.100 % without increasing the amount of production inputs and because of the optimal use of resources.
The average managerial efficiency has been obtained at 0.979 in this study. In other words, productivity can be increased up to 2.100 % .It can be conducted using the correct management techniques and motivation of the staff in MRDs of the hospitals without changing the amount of inputs. Therefore, effective steps can be taken to improve the productivity of MRDs in these hospitals by proper management, using the opinions of staff, and creating favorable working environments.
The average scale efficiency was 0.979 in this study. This means that an annual average of 2.100 % can be added to the output of MRDs in the studied hospitals. This is because of the savings caused by providing services on a large scale. Therefore, departments with increasing returns to scale should increase the level of providing services due to economic justification. Moreover, departments with decreasing returns to scale should review the overall structure of their department and adjust their capital and additional personnel inputs to avoid negative marginal production.
The main reason for decreased total factor productivity can be the lack of sufficient knowledge of the personnel in utilizing the existing equipment and technologies of this department for providing services in the right way. Therefore, training courses should be provided for the correct use of the equipment by personnel in departments, where the main reason for the decreased productivity is technological changes. In this study, the average annual output of MRDs has been reduced by 14.200 % due to technological changes. According to the results of Malmquist index, the range of changes in total factor productivity of MRDs of the studied hospitals in the review period was between 0.866 and 2.880. Therefore, productivity has increased only in 7 departments out of 20 and has decreased in another 13 departments. Therefore, high efficiency departments can be considered a model for other departments in terms of using production factors to increase efficiency and productivity.
In this regard, effective measures such as quantitative and qualitative improvement of providing services, continuous performance appraisal, and the optimal use of personnel and equipment of departments to increase the efficiency of hospital MRDs were proposed. Moreover, by continuously monitoring the performance of MRDs, the results can be used for planning and policy-making and avoiding wasting resources. The causes of their progress or decline can be determined by examining trends in total productivity changes. According to the results of the indexes calculated in this study, the authors can identify the amount of total productivity changes and its trend in MRDs of hospitals. Therefore, it is suggested that managers pay special attention to these methods to improve their productivity and performance.
Most of the studies on the productivity of total factor production in the health system have focused on the medical departments. So far, only one domestic study has been conducted on the productivity of MRDs at Tehran University of Medical Sciences through the Malmquist index. There have been no studies for the researchers to compare them with the results of this study. Therefore, the main limitation of this study was the impossibility of comparing the results of the present study with other studies. This research is the only study investigating the total factor productivity of all MRDs. It used two indexes of Malmquist and Kendrick-Creamer, which is considered its most significant strength compared to the study conducted by Dargahi et al. (10) They investigated changes in the productivity of the MRDs of Tehran University of Medical Sciences hospitals through the years 2006-2007. Assuming maximization of the production factors, they used the DEA method (Malmquist index), and calculated total productivity changes in their study. It was equal to 0.938. This number indicates that the productivity of MRDs in hospitals has decreased during the studied period due to the wrong assumption adopted to calculate the amount of productivity changes. Moreover, technological and technical efficiency changes had the highest effect on reducing the amount of total productivity changes. Changes in managerial efficiency and scale efficiency were in the next ranks, respectively (10). This was consistent with the results of this study. In general, the health system cannot control the number of patients referred to hospitals; thus, it is wrong to use the assumption of output maximization in calculations. Nouraei Motlagh et al. (19), in a study, investigated changes in the total factor productivity in hospitals affiliated with Lorestan University of Medical Sciences in 2010-2016. They used the DEA method for this purpose. In this study, the average total productivity change of hospitals during the studied period was 1.023. This indicates that productivity has decreased during the studied period, and technological changes had the maximum negative effect on productivity reduction compared to other factors (19). This is consistent with the results of this study. Furthermore, technological changes in the studies by Torabipour in Ahvaz hospitals (22), Krigia in Angola hospitals (23), and Yawe in Uganda hospitals (24) were the main cause of decreased total productivity, which is consistent with the results of the present study. Productivity of all departments in the hospital can be increased by upgrading technology and using the up-to-date equipment.
Conclusion
In this study, insufficient knowledge of personnel's MRD in the correct use of technology for providing services was the leading cause of decreased productivity. Therefore, providing instructions for correct use of technology can be helpful for personnel. The results of the Kendrick-Creamer and Malmquist indices can help managers improve productivity, and thus, reduce the costs of hospitals' medical records departments.
Acknowledgements
The authors would like to thank MRDs’ managers for their collaboration in data gathering.
Conflict of interests
Authors declared no conflict of interests.
Authors' contributions
Mokhtari A and Yusefzadeh H designed research; Mokhtari A, Nabilou B, Aghlmand S and Yusefzadeh H conducted research; Yusefzadeh H analyzed data; and Nabilou B and Mokhtari A wrote the paper. Yusefzadeh H had primary responsibility for final content. All authors read and approved the final manuscript.
Funding
This study was supported by Urmia University of Medical Sciences.
Type of Study: Original article |
Subject:
Health Economics
Received: 2022/02/26 | Accepted: 2022/05/20 | Published: 2022/07/3
Received: 2022/02/26 | Accepted: 2022/05/20 | Published: 2022/07/3
References
1. Khayeri F, Goudarzi L, Meshkini A, Khaki A. Implementation of "reducing the outpatient payments" program in hospitals. National Conference of the eleventh governments performance review in the field of health. Ministry of Health and Medical Education, Tehran, Iran. Tehran; May 5-6 2015; p. 12-3. [In Persian]
2. Ghaderi H, Goudarzi Gh, Gohari MR. Determination technical efficiency of hospitals affiliated with Iran University of Medical Science by data envelopment analysis (2000-2004). Journal of Health Administration. 2007; 9(26): 39-44.
3. Rezapour A, Ebadifard Azar F, Yousefzadeh N, Roumiani Y, Bagheri Faradonbeh S. Technical efficiency and resources allocation in university hospitals in Tehran, 2009-2012. Medical Journal of the Islamic Republic of Iran. 2015; 29(1): 839-50.
4. Hadian M, Rahimi B, Valinejadi A, Yusefzadeh H, Faghisolouk F. An analysis of productivity in hospitals affiliated to Iran and Tehran Universities Of Medical Sciences: 2006-2011. Journal of Health Administration. 2015; 17(58): 72-84. [In Persian]
5. Rahimi H, Khammar-nia M, Kavosi Z, Eslahi M. Indicators of hospital performance evaluation: A systematic review. International Journal of Hospital Research. 2014; 3(4): 199-208.
6. Nghiem S, Coelli T, Barber S. Sources of productivity growth in health services: A case study of Queensland public hospitals. Economic Analysis and Policy. 2011; 41(1): 37-48. [DOI:10.1016/S0313-5926(11)50003-7]
7. Raeisi AR, Yarmohammadian M, Mohammadi Bakhsh R, Gangi H. Performance evaluation of Al-Zahra academic medical center based on Iran balanced scorecard model. Journal of Education and Health Promotion. 2012; 1(1): 1. [DOI:10.4103/2277-9531.94408]
8. Yusefzadeh H, Ghaderi H, Bagherzade R, Barouni M. The efficiency and budgeting of public hospitals: Case study of Iran. Iranian Red Crescent Medical Journal. 2013; 15(5): 393-9. [DOI:10.5812/ircmj.4742]
9. Ajami S, Ketabi S, Torabiyan F. Performance improvement indicators of the medical records department and iInformation technology (IT) in hospitals. Pakistan Journal of Medical Sciences. 2015; 31(3): 717-20. [DOI:10.12669/pjms.313.8005]
10. Dargahi H, Masoori N, Safdari R, Fazaeli S, Yousefi M. Investigating productivity changes in medical records departments of Tehran University of Medical Sciences hospitals using malmquist index. Health Information Management. 2011; 8(3): 395-404. [In Persian]
11. Kuntz L, Scholtes S, Vera A. Incorporating efficiency in hospital-capacity planning in Germany. The European Journal of Health Economics. 2007; 8(3): 213-23. [DOI:10.1007/s10198-006-0021-6]
12. Emami Meybodi A. Measurement principles of efficiency and productivity. Second Edition. Tehran: Institute for Trade Studies and Research; 2005. [In Persian]
13. Li N-N, Wang C-H, Ni H, Wang H. Efficiency and productivity of county-level public hospitals based on the data envelopment analysis model and Malmquist index in Anhui, China. Chinese Medical Journal. 2017; 130(23): 2836-43. [DOI:10.4103/0366-6999.219148]
14. Mehregan MR. Data envelopment analysis: quantitative models in organizational performance evaluation. Tehran, Iran: Ketabedaneshgahi Publications; 2014. [In Persian]
15. Mujasi PN, Asbu EZ, Puig-Junoy J. How efficient are referral hospitals in Uganda? A data envelopment analysis and tobit regression approach. BMC Health Services Research. 2016; 16: 230. [DOI:10.1186/s12913-016-1472-9]
16. Nabilou B, Yusefzadeh H, Rezapour A, Ebadi Fard Azar F, Salem Safi P, Sarabi Asiabar A, et al. The productivity and its barriers in public hospitals: Case study of Iran. Medical Journal of the Islamic Republic of Iran. 2016; 30 (1): 36-43.
17. Silwal PR, Ashton T. Productivity of public hospitals in Nepal: A data envelopment analysis. BMJ Open. 2017; 7(7): e015327. [DOI:10.1136/bmjopen-2016-015327]
18. Valadkhani A, Dudu Moffat B, Harvie Ch. Malmquist indices of productivity change in Botswana's financial institutions. Global Business and Economics Review. 2009; 11(1): 28-43. [DOI:10.1504/GBER.2009.025380]
19. Nouraei Motlagh S, Ghasempour S, Yusefzadeh H, Lotfi F, Astaraki P, Saki K. Evaluation of the productivity of hospitals affiliated to Lorestan University of Medical Sciences using the malmquist and the kendrick-creamer indices. Shiraz E Medical Journal. 2019; 20(7): e85222. [In Persian] [DOI:10.5812/semj.85222]
20. Dargahi H, Masuri N, Safdari R, Fazaeli S, Yousefi M. The efficiency analysis of medical records departments of Tehran University of Medical Sciences hospitals with data envelopment analysis (2007-2009). Journal of Payavard Salamat. 2010; 4 (2 and 1) :9-17. [In Persian]
21. Sahin I, Ozcan YA, Ozgen Narci H. Assessment of hospital efficiency under health transformation program in Turkey. Central European Journal of Operations Research. 2009; 19(1): 19-37. [DOI:10.1007/s10100-009-0121-3]
22. Torabipour A, Bahmani T. Efficiency and productivity analysis of schools in Ahvaz University of Medical Sciences during 2011-2015. Journal of Medical Education Development. 2018; 11(31): 30-42. [In Persian] [DOI:10.29252/edcj.11.31.30]
23. Kirigia JM, Emrouznejad A, Cassoma B, Zere E, Barry S. A performance assessment method for hospitals: The case of municipal hospitals in Angola. Journal of Medical Systems. 2009; 32(6): 509-19. [DOI:10.1007/s10916-008-9157-5]
24. Yawe BL. Total factor productivity growth in Uganda's district referral hospitals. Tanzanian Economic Trends, TET: A Biannual Review of the Economy; 2006; 19(2): 26-42.
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |