Volume 7, Issue 1 (3-2023)
EBHPME 2023, 7(1): 13-24 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Alimoradnori M, Aghaei Hashjin A, Karami B. Policy Analysis of Retention of Physicians in Deprived Areas in Iran Using a Framework of Policy Analysis Triangle. EBHPME 2023; 7 (1) :13-24
URL: http://jebhpme.ssu.ac.ir/article-1-413-en.html
URL: http://jebhpme.ssu.ac.ir/article-1-413-en.html
Department of Health Services Management, School of Health Management and Information Sciences, Iran University of Medical Sciences, Tehran, Iran , aghaei.a@iums.ac.ir
Full-Text [PDF 1400 kb]
(1071 Downloads)
| Abstract (HTML) (1424 Views)
Full-Text: (242 Views)
A B S T R A C T
Background: The retention of physicians' policy is recommended by the World Health Organization (WHO) to achieve the goals of the health system and justice in access to health services. The aim of this study was policy analysis of retention of physicians in deprived areas and providing some recommendations for improvement of this plan.
Methods: This was a qualitative study regarding policy which used Walt and Gilson's triangle framework and Kingdon's multiple streams. Data were collected using a deep semi-structured interview with 30 participants and a review of upstream laws and regulations. After that, all the interviews were recorded, transcribed, and reviewed. Then, data were analyzed through MAXQDA/12 and content analysis.
Results: The findings of this study were categorized according to the policy context, content, and process, and actors who played a significant role in designing and implementing this policy.
Conclusion: The policy of retaining physicians in rural areas requires the support of the majority of the country's political and health authorities, and providing infrastructure for health providers. This policy not only increases the quality of services, but also is effective in increasing the patients' access to healthcare services in deprived areas.
Key words: Policy analysis, Retention of physicians, Policy triangle framework, Iran
Introduction
The health workers, including 10 % of the government's total employment and healthcare staff, are the backbone of health organizations. Unfair distribution of medical staff within countries leads to problems such as shortages of physicians in rural and deprived areas, which leads to reduced public access. Physicians play a vital role among medical staff, and their migration from deprived areas has created major concerns for health policymakers. Overall, about half of the world's population lives in deprived areas, served by a quarter of physicians and less than a third of the world's nurses. Retaining physicians in rural and deprived areas is a big challenge which jeopardizes an equal access and the quality and quantity of services provided. This problem exists in many countries, especially in middle and low-income ones (1-4). The imbalance of geographical distribution and the low number of health professionals is called global health worker crisis. This problem has increased since the 1990s due to the budget deficits in the health sector, demographic and epidemiological changes, and migration regarding the world's population (5). On the other hand, factors such as distance from the city center, low income, unfavorable weather conditions, poor health care system, lack of supervision, and lack of equipment and infrastructure affect migration from deprived areas (6, 7). Furthermore, this problem contributed to poor nutrition, the prevalence of chronic diseases, and increased harm and death among rural population more than urban ones (8). Some ways to solve this problem are monetary incentives
and giving loans to physicians in rural areas.
The WHO has proposed recommendations in four main categories: Training, regulations, financial incentives, and professional and personal support for health workers in deprived areas. Moreover, in 2010, the WHO published global policy recommendations for the retention of physicians in deprived areas. They include targeted admission for rural students, compulsory service in rural areas for new physicians, high financial incentives to work in villages, monetary incentives, giving loans to physicians, and prioritizing the acceptance of specialized training for physicians with experience regarding rural services (9-12). In South Africa, about 46 % of the population lives in deprived areas, but doctors constitute 12 % of the population. The rate of foreign physicians working in the United States and the United Kingdom is also around 25 and 27 %. These results indicate that high-income countries may have a shortage of specialists in rural areas (12). In addition, the results of Canada's census in 2016 revealed that about 18 % of the population lives in rural areas, but 8.2 % of Canadian physicians work outside of urban areas (7,13). In Iran, according to the law in 1988, medical and paramedical graduates are required to serve for the first year in rural areas. Health system reforms were followed in 2014, and the retention of physicians in deprived areas started on June, 2014 as part of the health system transformation plan (14). On the other hand, one of the main priorities of Iran’s Ministry of Health and Medical Education (MOHME) is to provide services to deprived and rural areas and three thousand specialists and sub-specialists serve in deprived areas of the country. However, the country faces the challenge of manpower shortage in this area. The Islamic Republic of Iran is facing a shortage of approximately 2,000 general practitioners and 1,700 specialists to provide services in deprived and rural areas (15, 16). Ministerial instructions and circulars have a significant impact on the density of physicians in the cities of Iran. Currently, there are no comprehensive and appropriate method for allocating human resources based on real needs, and the allocation of human resources is mostly based on traditional methods, which contributed to ignoring many basic needs of population (17). Therefore, the purpose of this study is to analyze the current policies regarding retention of physicians in Iran’s deprived areas to achieve an insight about the current policy process, identify influential factors in policymaking, evaluate their impact, and detect lessons learned to reform policies in the future.
Materials and Methods
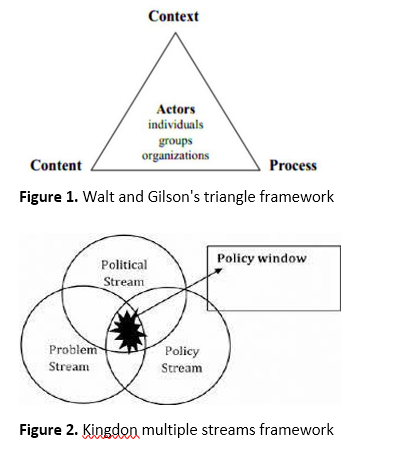
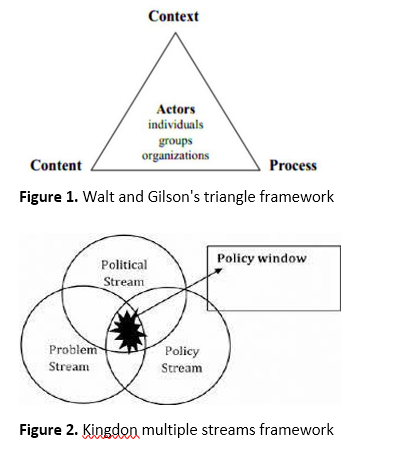
This was a qualitative study, with a deductive and a retrospective approach in the form of policy analysis. The policy of retaining physicians in deprived and rural areas was examined using Walt and Gilson's triangle framework. Walt and Gilson (1994) developed a framework for policy analysis which includes the context, actors, process, and content concepts (Figure 1). Actors are a collection of individuals, groups, and organizations involved in the implementation of a policy. Context includes social, economic, international, and political factors affecting a policy. Content refers to policy goals and planned actions. Process refers to actions taken during a policy (18). In addition, the Kingdon multiple streams framework (1984) was used for more analysis of the physician retention policy process in deprived and rural areas of Iran (Figure 2). In the theory of multiple streams, Kingdom argues that the public policy process consists of three streams: Problem stream, policy stream, and political stream. Problem stream includes the main problems societies face. A policy stream is an alternative policy that researchers and other stakeholders suggest to resolve problems. Political stream includes political transitions, national moods, elections, and pressure from interest groups. Regarding this framework, when a "policy window" opens, the three streams intersect and force governments to act (19).
Part of this study was policy documents (high-level documents and law, minutes, rules, regulations, plans, reports, articles, news, meeting statements, and lectures) related to the Health Transformation Plan in Iran. Sampling was done and all valid documents were collected through review of literature. Another part of this study was interviews with general practitioners (7 people) and specialists involved in the policy and working in deprived areas (5 people), faculty members (3 people), trustees of the plan for retention of physicians in deprived areas (5 people) and experts and experienced people in this field (10 people) in Tehran province in 2022. The number of interviewees was 30 participants. The authors used the purposeful sampling method until data saturation was met, and participants in this study introduced the next experts to the researcher. Interviews were recorded and then transcribed for analysis. Before data collection, the researcher provided the participants with study goals and methods and ensured the confidentiality of information. Scholars explained to the participants that participation in the study was voluntary. All the participants were required to sign informed consent forms to enter the study, and data were collected through semi-structured interviews. The interview contained two questions: 1): Please tell us about the policy of retaining of physicians in deprived areas? 2): Please tell us about the effective factors on retention policy regarding physicians in deprived areas?. The average interview duration was 45 to 75 minutes at workplace. The authors used qualitative research and content analysis method. Content analysis method was used for subjective interpretation. It is very suitable for extraction of concepts and meanings, and, systematic classification, coding or designing patterns are specified through this method. Validity in qualitative studies means that what the interviewer considers a finding is the same as what the participant has in mind, which is called credibility. Reliability in qualitative studies is the repeatability of data by other researchers (20). To confirm the validity, several pilot interviews were conducted, and the feedback was given to the participants after implementation; thus, the validity was confirmed. For the reliability of the interviews, pilot interviews were reviewed by the researcher, supervisors, and counselors and evaluated for repeatability results; hence, reliability of the interview was confirmed. Then, data were analyzed using the analytical software MAXQDA/12 and content analysis. The data obtained from documents were collected through literature review and interviews were analyzed using the MAXQDA software and content analysis method. After that, the collected data were classified into four categories of context, actors, process, and content using the Walt and Gilson triangle.
Results
Descriptive analysis of participants
The participants' demographic information included gender, work experience, and age category. The findings showed that 60 % of the participants were men, 44 % had work experience of about 26- 30 years, and most of them were in the age group of 46-50 (Table 1).
Walt and Gilson's triangle analysis
The findings of this study based on Walt and Gilson's triangle framework were categorized into four main dimensions: actors, content, context, and process.
Actors analysis
Actors dimension was divided into two categories: intra-organizational and extra-organizational factors. Intra-organizational factors included Ministry of Health and Medical Education (MOHME(, family physicians, association of specialists, Universities of Medical Sciences, Iran Health Insurance Organization and Social Security Insurance Organization, and Food and Drug Administration. Extra-organizational factors included villagers and residents of deprived areas, Planning and Budget Organization, the parliament of Iran, Medical Council of the Islamic Republic of Iran, World Bank, Ministry of Cooperation Labor and Social Welfare, Judiciary, Islamic Republic of Iran Broadcasting, local institutions such as Dispute Resolution Council, Supreme Council of Health and Food Security, medical system organization, WHO, Imam Khomeini Relief Foundation and Government (Table2).
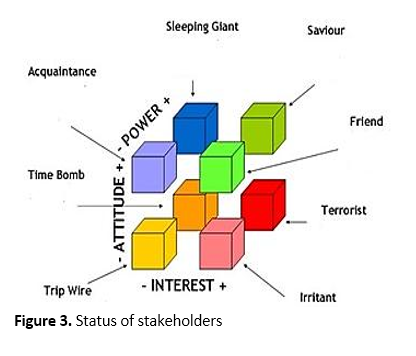
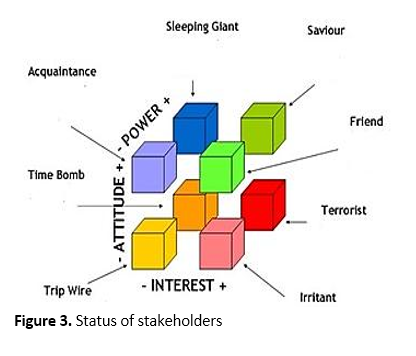
The stakeholder analysis matrix consists of 3 dimensions: 1. Power; it is the ability of stakeholders to influence the organization. This ability is due to the use of their position or resources in the organization. 2. Interest; this is the tendency of stakeholders in a project or program based on whether the project is active or inactive. 3. Attitude; it regards the attitude of stakeholders toward a project or program which is measured by the degree of support or blocking. These three dimensions include eight situations in stakeholder matrix analysis: 1. Savor; it refers to a powerful, positive attitude, high interest and influential, active and supportive people. Researchers must pay attention to these people and their needs and keep them on the team. 2. Friend; these people have low power, high interest, attitude, are active, and supportive. These people should be considered confidential. 3. Saboteur, these people have high power, a negative or intermittent attitude, are active. People must be prepared regarding their sabotage. 4. Irritant; these people have low power, high interest, a negative attitude, active. They must be involved even if they want to give up politics. 5. Sleeping giant; they have high power, low interest, positive and effective attitude, are passive, supportive. These people must be involved in politics. 6. Acquaintance; they have low power, low interest, and positive attitude but are insignificant, passive, and supportive. These people just need to be informed about politics. Time bomb; these people have high power, low interest, negative and influential attitude, are passive. They must be understood during policymaking before it is too late. Tripwire, such people have low power and, low interest, a negative attitude, are inactive. These people must be understood during the implementation
of the policy to prevent its failure (Figure 3) (Table3) (21).
Content analysis
In 2008, the WHO defined three goals for health systems: improving the level of health, responding to the non-medical needs of people, and fair financial participation. In Iran, the policy of retention of physicians in deprived areas started in 2014. This policy follows the general missions and upstream documents, Iran's 20-year vision plan, the general policies announced by the supreme leader, the laws related to health in the fifth strategic development plan, and the eleventh development program to improve the quality of health services in deprived and rural areas, increasing justice in access to services and health care up to the second and third levels, retention of physicians in villages, reduction of out-of-pocket payments to about 1 %, organizing the referral system, the removal of informal payments was implemented. In this policy, physicians have commitments such as not having a medical activity in clinics, surgery centers, private, charitable, and non-governmental hospitals. Moreover, physicians should be on-call 24 hours even during holidays and not receive any informal payment from patients (14, 22).
Context analysis
The effective factors on the policy of retaining physicians in deprived areas are classified into two macro-level factors and intra-sectoral factors categories (Table 4).
Political factors
These factors originated from the recommendations of the top leadership, considering the political conditions of the country during the period of sanctions, and finally, the change of government.
International factors
These factors were developed according to the goals of WHO such as health for all, universal health coverage, justice in access to health services in deprived areas, and reducing the-out-of pocket money.
Legal factors
These factors include the upstream documents of the country, paragraph "B" of article 34 in the fifth strategic development plans, paragraph "A" of article 36 in the fifth strategic development plans, paragraphs "7-9" of the macro policies of the health sector announced by the supreme leader, enactment number 74450/50982 dated 23/9/2014 of the council of ministers, and Iran's 20-year vision plan which focused on health and quality of life.
Economic factors
Some influential economic factors are high inflation in the country, financial constraints of people in deprived areas, the access of people to health services in rural areas, and high costs of traveling.
Structural factors
Weakness in the implementation of approved programs and lack of suitable facilities are the most important structural factors in the establishment and correct implementation of this policy. One of the participants said: “After being approved, this plan like thousands of other plans, had problems in the correct implementation phase. Unfortunately, recently, the response of the Ministry of Health to resolve the distribution of medical workers is to pay money to them for going to deprived areas. This is while some structural factors such as weakness in physical infrastructure, dilapidated buildings, insufficient medical equipment, and inappropriate facilities for living for medical forces were forgotten” (P5).
Social factors
Some of the problems of this policy not only include communication in the new society and environment but also the difficulty of commuting to the city and missing family and friends. All these cases are caused by the cultural differences between the physicians and the people of the deprived area. One of the participants said: “Imagine, I am a doctor from Tehran and provide services to rural areas in Sistan and Baluchestan province, I have to travel by land for about 15 hours. After arriving at my workplace, I will meet new people with a new language” (P7).
Cultural factors
Indigenization of physicians in deprived areas is one of the cultural issues. Because a physician lives in Tehran, the possibility of his retention in deprived areas should be considered based on cultural factors. One of the participants said: “Indigenization was not considered in this policy, and it was not implemented well. Maybe if indigenization was done, the result would be something else. But now, after about 8 years, we want to increase the medical capacity base on indigenization in entrance exam” (P11).
Motivational factors
Gaining experience and providing service in rural areas, if accompanied by privileges, can be considered a motivation to work in these areas. One of the participants said: "One of the motivational factors of doctors is to raise the score of deprived areas for physicians” (P4).
Process analysis
According to Kingdon's theory, three types of streams have been involved in the retention of physicians in rural areas.
Agendum
Problems stream
The performance of the country's health system indicates that there are problems in providing services in rural and deprived areas. The density of physicians and medical staff after graduating in big cities has created a disturbance in the provision of services and fair distribution of diagnostic and treatment services to the residents of deprived areas. In the first years after the revolution, the recruitment of physicians from other countries, like Pakistan and India, prevented the recruitment of physicians in Iran and created an adverse effect. On the other hand, there was a problem in the fair redistribution of manpower. One of the participants said: “The recruitment of foreign doctors and their employment after the revolution of 1978 caused dependence on foreign countries. The lack of training of local doctors, and years of planning were needed to resolve this problem and finally, it affected people's access to health services in deprived areas” (P9).
Policy stream
After paying attention to the public health principles of the Alma-Ata conference in 1978, paying attention to Primary Health Care (PHC) in Iran improved health results in villages, but it was not enough. In 1988, the parliament approved of a law to provide services in rural areas. Based on that, graduates of health and medical fields were required to provide services in rural and deprived areas. In 2005, the family physician policy was started in the rural and deprived areas, and this policy continued in the next government. The eleventh plan pursued a series of plans to reform and revise the health system under the title of Health System Transformation Plan (HSEP) based on the fourth and fifth strategic development plans by the Ministry of Health (17). According to the evidence, among the 191 countries of the world, Iran ranked 96th regarding health level, 113th in health distribution, 100th in response level, 93rd in distribution of non-medical needs, 112th in fair participation in financing ,and finally 114th, in achieving the goals of the health system. In October 2013, for achieving Universal Health Coverage (UHC), several meetings by health officials were held. The first step was taken on the fifth of May, 2015 after obtaining the legal approvals, presenting the proposed packages, and reporting the final instruction (22). The retention policy of physicians in deprived areas was aimed at increasing the access of people living in the deprived areas. This plan was based on paragraph "B" of article 34 of the fifth strategic development plan and paragraph "A" of article 36 of the fifth strategic development plan. It was implemented in June 2014 (14).
Political stream
The provision of health services faced many problems in 2012 and 2013. After that, politicians, policymakers, and legislators prioritized solving these problems. They tried to consider the improvement of health indicators in their policies. In 2014, the new government implemented the HSEP for gaining people's satisfaction, reducing out-of-pocket payments and increasing access to health services. One of the participants said: “In 2012 and 2013, the out-of-pocket payments of the people increased and the new government had to find a solution for the satisfaction of people, especially in deprived areas. In 2014, the government implemented a big policy called HSEP for the satisfaction of people, but this policy was not successful” (P15).
Policy window
According to Kingdon's theory, the policy window is opened when the three streams (problems stream, policy stream, and political stream) meet. After that, policymakers start their work. One of the participants said: “According to the Kingdon streams, all the streams must intersect at one point. In 2014, the conditions of the society and all streams were concentrated in one point, so that HSEP was prioritized and implemented”. When one of the streams is less important, the policy window is closed. In this plan, because of the lack of sufficient resources, infrastructure, and COVID-19, managers and policymakers' attention were drawn to these facts. Accordingly, HSEP and the policy of retaining physicians in deprived areas were weak, and the policy window was closed. One of the participants said: “As you know, if one of the streams of Kingdon is not addressed, the whole policy will be destroyed. For example, the policy of retaining physicians in deprived areas was supported by the eleventh development plan, after a while, due to the lack of resources and COVID-19, it was removed from the government's agenda” (P20).
Codify
The Ministry of Health conducted studies for the implementation of the HSEP and its packages over a period of 6 months, and several meetings were held to implement this policy. Then, the number of packages, their titles, financing, and details, including the policy of retaining physicians in deprived areas, were determined. Upstream documents, Iran's 20-year vision plan, and the general policies announced by the supreme leader were involved in codifying and implementing the retention policy regarding physicians in deprived areas. One of the participants said: “I still have a problem with this issue, why was HSEP started, especially the policy of retaining physicians in deprived areas, without studies and using the experiences of other countries? Why didn't we consider approving this plan in the parliament without getting the budget line for it?” Another participant said: “Why didn't we start this plan as a pilot in several provinces, like the family physician plan? In my opinion, it was better to start this plan with a pilot for identifying defects” (P24).
Policy implementation
In 2014, Health System Transformation Plan was launched, and in the June of the same year, the policy of retaining physicians in deprived areas was also addressed. In this policy, a list of physicians in rural areas and on-call doctors was prepared as a preliminary of the plan. According to the related instructions, the cities of the country were divided into two categories: cities included in the plan and cities not included in the plan. The covered areas were classified into four categories A, B, C, and D, each category including a special support package for physicians. Two types of incentive payments were considered to support the permanence of physicians in deprived areas: 1. Fixed payment: this is for A and B areas for general practitioners and specialists. Moreover, these payments are for A, B, C, and D areas for general practitioners who work in pre-hospital emergency.2. Performance payments: this payment is the increase of the K factor for A, B, C, and D areas. When the doctors accepted the obligations of the instructions and completed the relevant form, they were called covered physicians. In the next step, the completed forms were uploaded to the HSEP system. The treatment deputy of the health department was responsible for confirming the information. Physicians in deprived areas have obligations such as 24-hour presence in the city where they work. In the morning shift in the hospital clinic, in the afternoon shift in the special clinic, and at night, physicians should be on-call. The number of incentive payments was categorized based on indicators such as the degree of deprivation of the regions, weather classification, border or non-border regions, the population of the regions, and the score related to the social, economic, and cultural conditions. One of the participants said: “As a doctor, one of my main problems is that the Ministry of Health sees the solution of all problems in payments. For example, a doctor works in Ilam region. Can we solve all the deprivation and lack of facilities in deprived areas with money?” (P18).
Policy evaluation
The evaluation of the policy was planned at three international, national, and provincial levels. International level: Evaluation was done by a group of experts from the WHO. National level: Evaluation was done by the central headquarters in the Ministry of Health. Provincial level: The special supervision committee in universities of medical sciences and the executive committee were responsible for the evaluation, and experts used checklists for evaluation. There are several points in these evaluations. The first point is that the monitoring structures and the preparation of evaluation checklists for the environmental evaluation of this policy were not enough. The second point was the lack of sufficient, experienced, and specialized human resources to evaluate this policy. The third point addressed the performance status after of the policy and did not consider cost-effectiveness, cost-efficiency, and cost-opportunity (22). One of the participants said: “Perhaps the best sign of failure in the evaluation of this plan was that no results or reports of the successes or failures were published.” (P28).
Table 1. Descriptive analysis of participants
Table 2. The characteristics of stakeholders
Table 3. The status of stakeholders in the implementation of the policy regarding retaining physicians in deprived areas
Table 4. Effective factors on the policy of retaining physicians
Discussion
Recruitment and retention of physicians in rural areas is a big problem around the world. About half of the world's population lives in rural areas, while only a quarter of physicians cover this population. On the other hand, it is estimated that 1 billion people do not have access to PHC (2). This study examined the policy of retaining physicians in deprived areas of Iran using Walt Gilson's policy triangle. The results indicated that the important factors of this policy are divided into four categories: actors, content, process, and context. Liu X et al (23), examined the contextual factors in compulsory and incentive strategies for improving the attraction and retention of health workers in remote areas. The context of policy should be provided, otherwise, there will be problems all the time. The effects of the contextual conditions in their research were in line with the results of this study. In their study, Sajadi et al. (22) divided contextual conditions into general and specific categories. The general category included legal factors, upstream documents, Iran's 20-year vision plan, and the general policies announced by the supreme leader, all of which indicate legal considerations of the mentioned policy. In addition, the desire of political leaders and managers to implement policy is another important factor for this policy, which was in line with the results of this study. Koike et al. (24), examined retention among full-time occupational physicians in Japan. Flores et al. (25), studied the factors affecting retention in the Philippines. They showed that the retention rate of physicians in deprived areas was based on some factors such as the job promotion, social relationship between medical personnel, social support systems, competitive rewards, and job enrichment were increased. This was consistent with the results of this study. In a study, Ogundeji et al. (26) addressed recruitment and retention in Alberta rural area. Some of the main factors of physician recruitment and retention were: family and personal factors (long distance from family), social factors (communication with people), and motivational factors (financial incentives in rural areas). The results were in line with the ones in this study. Bashar et al. (27) discussed rethinking the policy of retaining doctors in a contracted-out primary healthcare setting in urban Bangladesh, and the many factors on the retention of doctors in deprived areas. On top of that, motivational factors such as financial incentives were mentioned as the most important factors, which were consistent with the results of this study. Morken et al. (28) examined factors influencing retention of rural physicians; the greatest factors which impact the retention of doctors in deprived areas included social relations, work environment, infrastructures, and work-life balance. This was consistent with the results of this study. They considered loan payment and educational opportunities as the least influential factors, which were not in line with the results of this study. Physicians who work in deprived areas should not work in the private sectors. Asefzadeh et al. (29) examined the factors influencing physicians' retention in teaching hospitals. They stated that physicians prefer to work in deprived and rural areas with the following conditions: proximity to the family, permission to work in the private sector, and access to clinical infrastructure. In fact, this study regards them as effective factors in the retention of physicians, being consistent with the results of this study. Amiresmaili et al. (30) studied the retention of dental practitioners in rural health services in Iran. They concluded that some personal and professional factors including age, marital status, age of the first child, type of contract, and work experience were effective in dentists' desire to stay in remote areas. In addition, some professional characteristics including dentists' life experience in rural areas and their families' attitudes toward living in such places influenced their willingness to stay. The correct distribution of human resources is one of the main factors in the retention of physicians and paramedics. Davari et al. (31) examined incentive policies for the retention of physicians and nurses in deprived areas. They revealed that the law regarding physicians and paramedics service delivery in deprived areas was effective and could solve the shortage of manpower in deprived areas. Considering limitations of this study, there was a lack of access to the participants due to the COVID-19 epidemic in special conditions.
Conclusion
One of the important factors for the success of any policy in the health system is paying attention to service providers, especially doctors, which, if ignored, will seriously damage the quality of health services. This policy requires the special attention of the authorities to infrastructure, welfare facilities, and solving the livelihood problems of doctors and their families. This leads to increased motivation and providing quality services; thus, increasing their retention in rural areas. Furthermore, the retention of doctors will reduce the costs of recruiting human resources, training, and preparation. The findings of this study can help relevant organizations to develop effective strategies and manage human resources.
Acknowledgements
The authors wish to express their appreciation to everyone who supported this study.
Conflict of interests
The authors declared no conflict of interests.
Authors' contributions
Aghaei Hashjin A and Alimoradnori M designed research; Aghaei Hashjin A and Karami B conducted research; Alimoradnori M and Karami B analyzed data; and Aghaei Hashjin A and Alimoradnori M wrote the manuscript. All the authors read and approved the final manuscript.
Funding
Non applicable.
Background: The retention of physicians' policy is recommended by the World Health Organization (WHO) to achieve the goals of the health system and justice in access to health services. The aim of this study was policy analysis of retention of physicians in deprived areas and providing some recommendations for improvement of this plan.
Methods: This was a qualitative study regarding policy which used Walt and Gilson's triangle framework and Kingdon's multiple streams. Data were collected using a deep semi-structured interview with 30 participants and a review of upstream laws and regulations. After that, all the interviews were recorded, transcribed, and reviewed. Then, data were analyzed through MAXQDA/12 and content analysis.
Results: The findings of this study were categorized according to the policy context, content, and process, and actors who played a significant role in designing and implementing this policy.
Conclusion: The policy of retaining physicians in rural areas requires the support of the majority of the country's political and health authorities, and providing infrastructure for health providers. This policy not only increases the quality of services, but also is effective in increasing the patients' access to healthcare services in deprived areas.
Key words: Policy analysis, Retention of physicians, Policy triangle framework, Iran
Introduction
The health workers, including 10 % of the government's total employment and healthcare staff, are the backbone of health organizations. Unfair distribution of medical staff within countries leads to problems such as shortages of physicians in rural and deprived areas, which leads to reduced public access. Physicians play a vital role among medical staff, and their migration from deprived areas has created major concerns for health policymakers. Overall, about half of the world's population lives in deprived areas, served by a quarter of physicians and less than a third of the world's nurses. Retaining physicians in rural and deprived areas is a big challenge which jeopardizes an equal access and the quality and quantity of services provided. This problem exists in many countries, especially in middle and low-income ones (1-4). The imbalance of geographical distribution and the low number of health professionals is called global health worker crisis. This problem has increased since the 1990s due to the budget deficits in the health sector, demographic and epidemiological changes, and migration regarding the world's population (5). On the other hand, factors such as distance from the city center, low income, unfavorable weather conditions, poor health care system, lack of supervision, and lack of equipment and infrastructure affect migration from deprived areas (6, 7). Furthermore, this problem contributed to poor nutrition, the prevalence of chronic diseases, and increased harm and death among rural population more than urban ones (8). Some ways to solve this problem are monetary incentives
and giving loans to physicians in rural areas.
The WHO has proposed recommendations in four main categories: Training, regulations, financial incentives, and professional and personal support for health workers in deprived areas. Moreover, in 2010, the WHO published global policy recommendations for the retention of physicians in deprived areas. They include targeted admission for rural students, compulsory service in rural areas for new physicians, high financial incentives to work in villages, monetary incentives, giving loans to physicians, and prioritizing the acceptance of specialized training for physicians with experience regarding rural services (9-12). In South Africa, about 46 % of the population lives in deprived areas, but doctors constitute 12 % of the population. The rate of foreign physicians working in the United States and the United Kingdom is also around 25 and 27 %. These results indicate that high-income countries may have a shortage of specialists in rural areas (12). In addition, the results of Canada's census in 2016 revealed that about 18 % of the population lives in rural areas, but 8.2 % of Canadian physicians work outside of urban areas (7,13). In Iran, according to the law in 1988, medical and paramedical graduates are required to serve for the first year in rural areas. Health system reforms were followed in 2014, and the retention of physicians in deprived areas started on June, 2014 as part of the health system transformation plan (14). On the other hand, one of the main priorities of Iran’s Ministry of Health and Medical Education (MOHME) is to provide services to deprived and rural areas and three thousand specialists and sub-specialists serve in deprived areas of the country. However, the country faces the challenge of manpower shortage in this area. The Islamic Republic of Iran is facing a shortage of approximately 2,000 general practitioners and 1,700 specialists to provide services in deprived and rural areas (15, 16). Ministerial instructions and circulars have a significant impact on the density of physicians in the cities of Iran. Currently, there are no comprehensive and appropriate method for allocating human resources based on real needs, and the allocation of human resources is mostly based on traditional methods, which contributed to ignoring many basic needs of population (17). Therefore, the purpose of this study is to analyze the current policies regarding retention of physicians in Iran’s deprived areas to achieve an insight about the current policy process, identify influential factors in policymaking, evaluate their impact, and detect lessons learned to reform policies in the future.
Materials and Methods
This was a qualitative study, with a deductive and a retrospective approach in the form of policy analysis. The policy of retaining physicians in deprived and rural areas was examined using Walt and Gilson's triangle framework. Walt and Gilson (1994) developed a framework for policy analysis which includes the context, actors, process, and content concepts (Figure 1). Actors are a collection of individuals, groups, and organizations involved in the implementation of a policy. Context includes social, economic, international, and political factors affecting a policy. Content refers to policy goals and planned actions. Process refers to actions taken during a policy (18). In addition, the Kingdon multiple streams framework (1984) was used for more analysis of the physician retention policy process in deprived and rural areas of Iran (Figure 2). In the theory of multiple streams, Kingdom argues that the public policy process consists of three streams: Problem stream, policy stream, and political stream. Problem stream includes the main problems societies face. A policy stream is an alternative policy that researchers and other stakeholders suggest to resolve problems. Political stream includes political transitions, national moods, elections, and pressure from interest groups. Regarding this framework, when a "policy window" opens, the three streams intersect and force governments to act (19).
Part of this study was policy documents (high-level documents and law, minutes, rules, regulations, plans, reports, articles, news, meeting statements, and lectures) related to the Health Transformation Plan in Iran. Sampling was done and all valid documents were collected through review of literature. Another part of this study was interviews with general practitioners (7 people) and specialists involved in the policy and working in deprived areas (5 people), faculty members (3 people), trustees of the plan for retention of physicians in deprived areas (5 people) and experts and experienced people in this field (10 people) in Tehran province in 2022. The number of interviewees was 30 participants. The authors used the purposeful sampling method until data saturation was met, and participants in this study introduced the next experts to the researcher. Interviews were recorded and then transcribed for analysis. Before data collection, the researcher provided the participants with study goals and methods and ensured the confidentiality of information. Scholars explained to the participants that participation in the study was voluntary. All the participants were required to sign informed consent forms to enter the study, and data were collected through semi-structured interviews. The interview contained two questions: 1): Please tell us about the policy of retaining of physicians in deprived areas? 2): Please tell us about the effective factors on retention policy regarding physicians in deprived areas?. The average interview duration was 45 to 75 minutes at workplace. The authors used qualitative research and content analysis method. Content analysis method was used for subjective interpretation. It is very suitable for extraction of concepts and meanings, and, systematic classification, coding or designing patterns are specified through this method. Validity in qualitative studies means that what the interviewer considers a finding is the same as what the participant has in mind, which is called credibility. Reliability in qualitative studies is the repeatability of data by other researchers (20). To confirm the validity, several pilot interviews were conducted, and the feedback was given to the participants after implementation; thus, the validity was confirmed. For the reliability of the interviews, pilot interviews were reviewed by the researcher, supervisors, and counselors and evaluated for repeatability results; hence, reliability of the interview was confirmed. Then, data were analyzed using the analytical software MAXQDA/12 and content analysis. The data obtained from documents were collected through literature review and interviews were analyzed using the MAXQDA software and content analysis method. After that, the collected data were classified into four categories of context, actors, process, and content using the Walt and Gilson triangle.
Results
Descriptive analysis of participants
The participants' demographic information included gender, work experience, and age category. The findings showed that 60 % of the participants were men, 44 % had work experience of about 26- 30 years, and most of them were in the age group of 46-50 (Table 1).
Walt and Gilson's triangle analysis
The findings of this study based on Walt and Gilson's triangle framework were categorized into four main dimensions: actors, content, context, and process.
Actors analysis
Actors dimension was divided into two categories: intra-organizational and extra-organizational factors. Intra-organizational factors included Ministry of Health and Medical Education (MOHME(, family physicians, association of specialists, Universities of Medical Sciences, Iran Health Insurance Organization and Social Security Insurance Organization, and Food and Drug Administration. Extra-organizational factors included villagers and residents of deprived areas, Planning and Budget Organization, the parliament of Iran, Medical Council of the Islamic Republic of Iran, World Bank, Ministry of Cooperation Labor and Social Welfare, Judiciary, Islamic Republic of Iran Broadcasting, local institutions such as Dispute Resolution Council, Supreme Council of Health and Food Security, medical system organization, WHO, Imam Khomeini Relief Foundation and Government (Table2).
The stakeholder analysis matrix consists of 3 dimensions: 1. Power; it is the ability of stakeholders to influence the organization. This ability is due to the use of their position or resources in the organization. 2. Interest; this is the tendency of stakeholders in a project or program based on whether the project is active or inactive. 3. Attitude; it regards the attitude of stakeholders toward a project or program which is measured by the degree of support or blocking. These three dimensions include eight situations in stakeholder matrix analysis: 1. Savor; it refers to a powerful, positive attitude, high interest and influential, active and supportive people. Researchers must pay attention to these people and their needs and keep them on the team. 2. Friend; these people have low power, high interest, attitude, are active, and supportive. These people should be considered confidential. 3. Saboteur, these people have high power, a negative or intermittent attitude, are active. People must be prepared regarding their sabotage. 4. Irritant; these people have low power, high interest, a negative attitude, active. They must be involved even if they want to give up politics. 5. Sleeping giant; they have high power, low interest, positive and effective attitude, are passive, supportive. These people must be involved in politics. 6. Acquaintance; they have low power, low interest, and positive attitude but are insignificant, passive, and supportive. These people just need to be informed about politics. Time bomb; these people have high power, low interest, negative and influential attitude, are passive. They must be understood during policymaking before it is too late. Tripwire, such people have low power and, low interest, a negative attitude, are inactive. These people must be understood during the implementation
of the policy to prevent its failure (Figure 3) (Table3) (21).
Content analysis
In 2008, the WHO defined three goals for health systems: improving the level of health, responding to the non-medical needs of people, and fair financial participation. In Iran, the policy of retention of physicians in deprived areas started in 2014. This policy follows the general missions and upstream documents, Iran's 20-year vision plan, the general policies announced by the supreme leader, the laws related to health in the fifth strategic development plan, and the eleventh development program to improve the quality of health services in deprived and rural areas, increasing justice in access to services and health care up to the second and third levels, retention of physicians in villages, reduction of out-of-pocket payments to about 1 %, organizing the referral system, the removal of informal payments was implemented. In this policy, physicians have commitments such as not having a medical activity in clinics, surgery centers, private, charitable, and non-governmental hospitals. Moreover, physicians should be on-call 24 hours even during holidays and not receive any informal payment from patients (14, 22).
Context analysis
The effective factors on the policy of retaining physicians in deprived areas are classified into two macro-level factors and intra-sectoral factors categories (Table 4).
Political factors
These factors originated from the recommendations of the top leadership, considering the political conditions of the country during the period of sanctions, and finally, the change of government.
International factors
These factors were developed according to the goals of WHO such as health for all, universal health coverage, justice in access to health services in deprived areas, and reducing the-out-of pocket money.
Legal factors
These factors include the upstream documents of the country, paragraph "B" of article 34 in the fifth strategic development plans, paragraph "A" of article 36 in the fifth strategic development plans, paragraphs "7-9" of the macro policies of the health sector announced by the supreme leader, enactment number 74450/50982 dated 23/9/2014 of the council of ministers, and Iran's 20-year vision plan which focused on health and quality of life.
Economic factors
Some influential economic factors are high inflation in the country, financial constraints of people in deprived areas, the access of people to health services in rural areas, and high costs of traveling.
Structural factors
Weakness in the implementation of approved programs and lack of suitable facilities are the most important structural factors in the establishment and correct implementation of this policy. One of the participants said: “After being approved, this plan like thousands of other plans, had problems in the correct implementation phase. Unfortunately, recently, the response of the Ministry of Health to resolve the distribution of medical workers is to pay money to them for going to deprived areas. This is while some structural factors such as weakness in physical infrastructure, dilapidated buildings, insufficient medical equipment, and inappropriate facilities for living for medical forces were forgotten” (P5).
Social factors
Some of the problems of this policy not only include communication in the new society and environment but also the difficulty of commuting to the city and missing family and friends. All these cases are caused by the cultural differences between the physicians and the people of the deprived area. One of the participants said: “Imagine, I am a doctor from Tehran and provide services to rural areas in Sistan and Baluchestan province, I have to travel by land for about 15 hours. After arriving at my workplace, I will meet new people with a new language” (P7).
Cultural factors
Indigenization of physicians in deprived areas is one of the cultural issues. Because a physician lives in Tehran, the possibility of his retention in deprived areas should be considered based on cultural factors. One of the participants said: “Indigenization was not considered in this policy, and it was not implemented well. Maybe if indigenization was done, the result would be something else. But now, after about 8 years, we want to increase the medical capacity base on indigenization in entrance exam” (P11).
Motivational factors
Gaining experience and providing service in rural areas, if accompanied by privileges, can be considered a motivation to work in these areas. One of the participants said: "One of the motivational factors of doctors is to raise the score of deprived areas for physicians” (P4).
Process analysis
According to Kingdon's theory, three types of streams have been involved in the retention of physicians in rural areas.
Agendum
Problems stream
The performance of the country's health system indicates that there are problems in providing services in rural and deprived areas. The density of physicians and medical staff after graduating in big cities has created a disturbance in the provision of services and fair distribution of diagnostic and treatment services to the residents of deprived areas. In the first years after the revolution, the recruitment of physicians from other countries, like Pakistan and India, prevented the recruitment of physicians in Iran and created an adverse effect. On the other hand, there was a problem in the fair redistribution of manpower. One of the participants said: “The recruitment of foreign doctors and their employment after the revolution of 1978 caused dependence on foreign countries. The lack of training of local doctors, and years of planning were needed to resolve this problem and finally, it affected people's access to health services in deprived areas” (P9).
Policy stream
After paying attention to the public health principles of the Alma-Ata conference in 1978, paying attention to Primary Health Care (PHC) in Iran improved health results in villages, but it was not enough. In 1988, the parliament approved of a law to provide services in rural areas. Based on that, graduates of health and medical fields were required to provide services in rural and deprived areas. In 2005, the family physician policy was started in the rural and deprived areas, and this policy continued in the next government. The eleventh plan pursued a series of plans to reform and revise the health system under the title of Health System Transformation Plan (HSEP) based on the fourth and fifth strategic development plans by the Ministry of Health (17). According to the evidence, among the 191 countries of the world, Iran ranked 96th regarding health level, 113th in health distribution, 100th in response level, 93rd in distribution of non-medical needs, 112th in fair participation in financing ,and finally 114th, in achieving the goals of the health system. In October 2013, for achieving Universal Health Coverage (UHC), several meetings by health officials were held. The first step was taken on the fifth of May, 2015 after obtaining the legal approvals, presenting the proposed packages, and reporting the final instruction (22). The retention policy of physicians in deprived areas was aimed at increasing the access of people living in the deprived areas. This plan was based on paragraph "B" of article 34 of the fifth strategic development plan and paragraph "A" of article 36 of the fifth strategic development plan. It was implemented in June 2014 (14).
Political stream
The provision of health services faced many problems in 2012 and 2013. After that, politicians, policymakers, and legislators prioritized solving these problems. They tried to consider the improvement of health indicators in their policies. In 2014, the new government implemented the HSEP for gaining people's satisfaction, reducing out-of-pocket payments and increasing access to health services. One of the participants said: “In 2012 and 2013, the out-of-pocket payments of the people increased and the new government had to find a solution for the satisfaction of people, especially in deprived areas. In 2014, the government implemented a big policy called HSEP for the satisfaction of people, but this policy was not successful” (P15).
Policy window
According to Kingdon's theory, the policy window is opened when the three streams (problems stream, policy stream, and political stream) meet. After that, policymakers start their work. One of the participants said: “According to the Kingdon streams, all the streams must intersect at one point. In 2014, the conditions of the society and all streams were concentrated in one point, so that HSEP was prioritized and implemented”. When one of the streams is less important, the policy window is closed. In this plan, because of the lack of sufficient resources, infrastructure, and COVID-19, managers and policymakers' attention were drawn to these facts. Accordingly, HSEP and the policy of retaining physicians in deprived areas were weak, and the policy window was closed. One of the participants said: “As you know, if one of the streams of Kingdon is not addressed, the whole policy will be destroyed. For example, the policy of retaining physicians in deprived areas was supported by the eleventh development plan, after a while, due to the lack of resources and COVID-19, it was removed from the government's agenda” (P20).
Codify
The Ministry of Health conducted studies for the implementation of the HSEP and its packages over a period of 6 months, and several meetings were held to implement this policy. Then, the number of packages, their titles, financing, and details, including the policy of retaining physicians in deprived areas, were determined. Upstream documents, Iran's 20-year vision plan, and the general policies announced by the supreme leader were involved in codifying and implementing the retention policy regarding physicians in deprived areas. One of the participants said: “I still have a problem with this issue, why was HSEP started, especially the policy of retaining physicians in deprived areas, without studies and using the experiences of other countries? Why didn't we consider approving this plan in the parliament without getting the budget line for it?” Another participant said: “Why didn't we start this plan as a pilot in several provinces, like the family physician plan? In my opinion, it was better to start this plan with a pilot for identifying defects” (P24).
Policy implementation
In 2014, Health System Transformation Plan was launched, and in the June of the same year, the policy of retaining physicians in deprived areas was also addressed. In this policy, a list of physicians in rural areas and on-call doctors was prepared as a preliminary of the plan. According to the related instructions, the cities of the country were divided into two categories: cities included in the plan and cities not included in the plan. The covered areas were classified into four categories A, B, C, and D, each category including a special support package for physicians. Two types of incentive payments were considered to support the permanence of physicians in deprived areas: 1. Fixed payment: this is for A and B areas for general practitioners and specialists. Moreover, these payments are for A, B, C, and D areas for general practitioners who work in pre-hospital emergency.2. Performance payments: this payment is the increase of the K factor for A, B, C, and D areas. When the doctors accepted the obligations of the instructions and completed the relevant form, they were called covered physicians. In the next step, the completed forms were uploaded to the HSEP system. The treatment deputy of the health department was responsible for confirming the information. Physicians in deprived areas have obligations such as 24-hour presence in the city where they work. In the morning shift in the hospital clinic, in the afternoon shift in the special clinic, and at night, physicians should be on-call. The number of incentive payments was categorized based on indicators such as the degree of deprivation of the regions, weather classification, border or non-border regions, the population of the regions, and the score related to the social, economic, and cultural conditions. One of the participants said: “As a doctor, one of my main problems is that the Ministry of Health sees the solution of all problems in payments. For example, a doctor works in Ilam region. Can we solve all the deprivation and lack of facilities in deprived areas with money?” (P18).
Policy evaluation
The evaluation of the policy was planned at three international, national, and provincial levels. International level: Evaluation was done by a group of experts from the WHO. National level: Evaluation was done by the central headquarters in the Ministry of Health. Provincial level: The special supervision committee in universities of medical sciences and the executive committee were responsible for the evaluation, and experts used checklists for evaluation. There are several points in these evaluations. The first point is that the monitoring structures and the preparation of evaluation checklists for the environmental evaluation of this policy were not enough. The second point was the lack of sufficient, experienced, and specialized human resources to evaluate this policy. The third point addressed the performance status after of the policy and did not consider cost-effectiveness, cost-efficiency, and cost-opportunity (22). One of the participants said: “Perhaps the best sign of failure in the evaluation of this plan was that no results or reports of the successes or failures were published.” (P28).
Table 1. Descriptive analysis of participants
| Variable | Frequency | percentage | |
| Sex | Man | 18 | 60 |
| Female | 12 | 40 | |
| Work experience | Under 20 | 12 | 40 |
| 20-25 | 5 | 16 | |
| 26-30 | 13 | 44 | |
| Age | Under 40 | 6 | 20 |
| 40-45 | 10 | 34 | |
| 46-50 | 14 | 46 | |
| attitude | power | interest | Actors' roles | Actors | |
| 5 | 5 | 5 | Policy maker | MOHME | Internal organizational |
| 3 | 1 | 1 | Service provider | Family physicians | |
| 1 | 3 | 1 | Service provider | Society of specialists | |
| 5 | 5 | 5 | Policy implementation | Universities of medical sciences | |
| 1 | 5 | 1 | Service buyer | Iran Health Insurance Organization and Social Security Insurance Organization | |
| 1 | 5 | 1 | supportive | Food and Drug Administration | |
| 5 | 1 | 5 | Services recipient | Villagers and residents of deprived areas, | Extra-organizational |
| 5 | 5 | 5 | Facilitator | Planning and Budget Organization | |
| 5 | 5 | 5 | Legislative | The parliament of Iran | |
| 5 | 1 | 5 | Supportive | Medical Council of the Islamic Republic of Iran | |
| 5 | 5 | 5 | Facilitator | World Bank | |
| 1 | 5 | 1 | Supportive | Ministry of Cooperatives, Labor and Social Welfare | |
| 1 | 5 | 1 | supportive | Judiciary | |
| 1 | 5 | 1 | Advertising | Islamic Republic of Iran Broadcasting | |
| 5 | 1 | 5 | Supportive | Local institutions such as: Dispute Resolution Council, Supreme Council of Health and Food Security | |
| 5 | 5 | 5 | Supportive | WHO | |
| 5 | 1 | 5 | Supportive | Imam Khomeini Relief Foundation | |
| 5 | 5 | 5 | Policy implementation | Government |
Table 3. The status of stakeholders in the implementation of the policy regarding retaining physicians in deprived areas
| Stakeholders | Status of stakeholders | Stakeholders categories |
| Villagers and residents of deprived areas, local institutions such as: : Dispute Resolution Council , Supreme Council of Health and Food Security, Imam Khomeini Relief Foundation, Medical Council of the Islamic Republic of Iran | High interest - high attitude - low power | Friend |
| Ministry of Health and Medical Education (MOHME) , Universities of Medical Sciences , Planning and Budget Organization , The Parliament of Iran , World Bank , WHO | High interest - high attitude - high power | Savior |
| - | Low interest - high attitude - low power | Acquaintance |
| - | Low interest - high attitude - high power | Sleeping giant |
| - | High interest - low attitude - low power | Irritant |
| - | Low interest - low attitude - low power | Tripwire |
| Food and Drug Administration, Ministry of Cooperation, labor and Social Welfare, Judiciary, Islamic Republic of Iran Broadcasting, Iran Health Insurance Organization and Social Security Insurance Organization | Low interest -low attitude-high power | Time Bomb |
| Family Physicians , Association of Specialists | High interest -low attitude -high power | Saboteur |
| Intra-sector factors | Macro- level factors |
| Structural | Political |
| Social | International |
| Cultural | Legal |
| Motivational | Economic |
Discussion
Recruitment and retention of physicians in rural areas is a big problem around the world. About half of the world's population lives in rural areas, while only a quarter of physicians cover this population. On the other hand, it is estimated that 1 billion people do not have access to PHC (2). This study examined the policy of retaining physicians in deprived areas of Iran using Walt Gilson's policy triangle. The results indicated that the important factors of this policy are divided into four categories: actors, content, process, and context. Liu X et al (23), examined the contextual factors in compulsory and incentive strategies for improving the attraction and retention of health workers in remote areas. The context of policy should be provided, otherwise, there will be problems all the time. The effects of the contextual conditions in their research were in line with the results of this study. In their study, Sajadi et al. (22) divided contextual conditions into general and specific categories. The general category included legal factors, upstream documents, Iran's 20-year vision plan, and the general policies announced by the supreme leader, all of which indicate legal considerations of the mentioned policy. In addition, the desire of political leaders and managers to implement policy is another important factor for this policy, which was in line with the results of this study. Koike et al. (24), examined retention among full-time occupational physicians in Japan. Flores et al. (25), studied the factors affecting retention in the Philippines. They showed that the retention rate of physicians in deprived areas was based on some factors such as the job promotion, social relationship between medical personnel, social support systems, competitive rewards, and job enrichment were increased. This was consistent with the results of this study. In a study, Ogundeji et al. (26) addressed recruitment and retention in Alberta rural area. Some of the main factors of physician recruitment and retention were: family and personal factors (long distance from family), social factors (communication with people), and motivational factors (financial incentives in rural areas). The results were in line with the ones in this study. Bashar et al. (27) discussed rethinking the policy of retaining doctors in a contracted-out primary healthcare setting in urban Bangladesh, and the many factors on the retention of doctors in deprived areas. On top of that, motivational factors such as financial incentives were mentioned as the most important factors, which were consistent with the results of this study. Morken et al. (28) examined factors influencing retention of rural physicians; the greatest factors which impact the retention of doctors in deprived areas included social relations, work environment, infrastructures, and work-life balance. This was consistent with the results of this study. They considered loan payment and educational opportunities as the least influential factors, which were not in line with the results of this study. Physicians who work in deprived areas should not work in the private sectors. Asefzadeh et al. (29) examined the factors influencing physicians' retention in teaching hospitals. They stated that physicians prefer to work in deprived and rural areas with the following conditions: proximity to the family, permission to work in the private sector, and access to clinical infrastructure. In fact, this study regards them as effective factors in the retention of physicians, being consistent with the results of this study. Amiresmaili et al. (30) studied the retention of dental practitioners in rural health services in Iran. They concluded that some personal and professional factors including age, marital status, age of the first child, type of contract, and work experience were effective in dentists' desire to stay in remote areas. In addition, some professional characteristics including dentists' life experience in rural areas and their families' attitudes toward living in such places influenced their willingness to stay. The correct distribution of human resources is one of the main factors in the retention of physicians and paramedics. Davari et al. (31) examined incentive policies for the retention of physicians and nurses in deprived areas. They revealed that the law regarding physicians and paramedics service delivery in deprived areas was effective and could solve the shortage of manpower in deprived areas. Considering limitations of this study, there was a lack of access to the participants due to the COVID-19 epidemic in special conditions.
Conclusion
One of the important factors for the success of any policy in the health system is paying attention to service providers, especially doctors, which, if ignored, will seriously damage the quality of health services. This policy requires the special attention of the authorities to infrastructure, welfare facilities, and solving the livelihood problems of doctors and their families. This leads to increased motivation and providing quality services; thus, increasing their retention in rural areas. Furthermore, the retention of doctors will reduce the costs of recruiting human resources, training, and preparation. The findings of this study can help relevant organizations to develop effective strategies and manage human resources.
Acknowledgements
The authors wish to express their appreciation to everyone who supported this study.
Conflict of interests
The authors declared no conflict of interests.
Authors' contributions
Aghaei Hashjin A and Alimoradnori M designed research; Aghaei Hashjin A and Karami B conducted research; Alimoradnori M and Karami B analyzed data; and Aghaei Hashjin A and Alimoradnori M wrote the manuscript. All the authors read and approved the final manuscript.
Funding
Non applicable.
Type of Study: Original article |
Subject:
Health Policy
Received: 2022/11/15 | Accepted: 2023/03/28 | Published: 2023/03/30
Received: 2022/11/15 | Accepted: 2023/03/28 | Published: 2023/03/30
References
1. Asghari Sh, Kirkland MC, Blackmore J, Boyd S, Farrell A, Rourke J, et al. A systematic review of reviews: Recruitment and retention of rural family physicians. Can J Rural Med. 2020; 25(1): 20-30. [DOI: 10.4103/CJRM.CJRM_4_19]
2. World Health Organization. Increasing access to health workers in remote and rural areas through improved retention: global policy recommendations. World Health Organization. Available from URL: http://apps.who.int/iris/ handle/10665/44369. Last access: 31 December, 2022.
3. Mohammadiaghdam N, Doshmangir L, Babaie J, Khabiri R, Ponnet K. Determining factors in the retention of physicians in rural and underdeveloped areas: A systematic review. BMC Fam Pract. 2020; 21(1): 216. [DOI: 10.1186/s12875-020-01279-7]
4. Rocha EMS, Boiteux PDA, de Azevedo GD, Siqueira CEG, Andrade MAC. Educational predictors for the retention of physicians in remote and unassisted areas: A narrative review. Revista Brasileira de Educação Médica . 2020; 44(01). [DOI: 10.1590/1981-5271v44.1-20190281]
5. Ehsani-Chimeh E, Majdzadeh R, Delavari S, Najafi Gharebelagh M, Rezaei S, Homaie Rad E. Physicians' retention rate and its effective factors in the Islamic Republic of Iran. East Mediterr Health J. 2018; 24(9): 830-7. [DOI: 10.26719/2018.24.9.830]
6. Lehmann U, Dieleman M, Martineau T. Staffing remote rural areas in middle- and low-income countries: A literature review of attraction and retention. BMC Health Serv Res. 2008; 8: 19. [DOI: 10.1186/1472-6963-8-19]
7. Larsen Soles T, Wilson CR, Oandasan IF. Family medicine education in rural communities as a health service intervention supporting recruitment and retention of physicians. Can Fam Physician. 2017; 63(1): 28-32.
8. Herbert R. Canada’s health care challenge: Recognizing and addressing the health needs of rural Canadians. Lethbridge Undergrad Res J. 2007; 2(1): 1-8.
9. Buchan J, Couper ID, Tangcharoensathien V, Thepannya Kh, Jaskiewicz W, Perfilieva G, Dolea C. Early implementation of WHO recommendations for the retention of health workers in remote and rural areas. Bull World Health Organ. 2013; 91(11): 834-40. [DOI: 10.2471/BLT.13.119008]
10. Kumar S, Clancy B. Retention of physicians and surgeons in rural areas-what works?. J Public Health. 2021; 43(4): e689-e700. [DOI: 10.1093/ pubmed/fdaa031]
11. Handoyo NE, Rahayu GR, Claramita M, Ash J, Schuwirth LWT. Personal resilience and rural doctors retention: A study in Indonesia. Rural Remote Health. 2020; 20(4): 6097. [DOI: 10.22605/ RRH6097]
12. Cortez LR, Guerra EC, da Silveira NJD, Noro LRA. The retention of physicians to primary health care in Brazil: Motivation and limitations from a qualitative perspective. BMC Health Serv Res. 2019 ; 19(1): 57. [DOI: 10.1186/s12913-018-3813-3]
13. Lafortune C, Gustafson J. Interventions to improve recruitment and retention of physicians in rural and remote Canada: A systematic review. UWOMJ. 2019; 88(1). [DOI: 10.5206/uwomj.v88i1.6184]
14. Vaezi H, Aghajani M, Rategar M, Shahrami A, Lotfi F, Olyaeemanesh A, et al. Implementing the healthtransformation plan with emphasis on supporting the survival of physicians in deprived areas: The results and challenges. Hakim Health Sys Res. 2017; 19(4): 238-47. [In Persian]
15. Emami Razavi SH, Shali M, Mirzaei S, Nikbakht Nasrabadi AR, Khazaeipour Z. Challenges of physicians working long in deprived areas in Iran. Payavard. 2021; 15(3): 224-34. [In Persian]
16. Mollaei B, Moghri J, Ghavami V, Tabatabaee SS. Factors related to the willingness of working physicians to stay in rural areas and their evaluation according to the recommendations of the World Health Organization: A case study. Journal of Health Administration. 2021; 23(4): 40-50. [In Persian] [DOI: 10.29252/ jha.23.4.40]
17. Davari F, Sajadi HS, Ehsani-Chimeh E, Alimohammadzadeh KH. Incentive policies for the retention of physicians and nurses in deprived areas of the Islamic Republic of Iran. Health Inf Manage. 2020; 17(4): 159-66. [In Persian]
18. Mehtarpour M, Tajvar M. Policy analysis of family physician plan and referral system in iran using policy analysis triangle framework. Health_Based Research. 2018; 4(1): 31-49. [In Persian]
19. Yousefinezhadi T, Mosadeghrad AM, Arab M, Ramezani M, Akbari Sari A. An analysis of hospital accreditation policy in Iran. Iran J Public Health. 2017; 46(10): 1347-58.
20. Keyvanara M, ShaarbafchiZadeh N, Alimoradnori M. Effective factors on occupational burnout among the operating room staff in teaching hospitals affiliated with Isfahan Medical University: A qualitative content analysis. EBHPME. 2019; 3(3): 202-11. [DOI: 10.18502/jebhpme.v3i3.1509]
21. Murray-Webster R, Simon P. Making sense of stakeholder mapping. PM World today. 2006; 8(11): 1-5.
22. Sajadi HS, Hosseini M, Dehghani A, Khodayari R, Zandiyan H, Hosseini SS. The policy analysis of Iran’s health transformation plan in therapeutic services. Hakim Health Sys Res. 2018; 21(2): 71-88. [In Persian]
23. Liu X, Dou L, Zhang H, Sun Y, Yuan B. Analysis of context factors in compulsory and incentive strategies for improving attraction and retention of health workers in rural and remote areas: A systematic review. Hum Resour Health. 2015; 13: 61. [DOI: 10.1186/s12960-015-0059-6]
24. Koike S, Isse T, Kawaguchi H, Ogawa M. Retention among full-time occupational physicians in Japan. Occup Med (Lond). 2019; 69(2): 139-42. [DOI: 10.1093/occmed/kqy130]
25. Flores ELL, Manahan EMR, Lacanilao MPB, Ladaw IMBT, Mallillin MMB, Mappatao NTQ, et al. Factors affecting retention in the Philippine National Rural Physician Deployment Program from 2012 to 2019: A mixed methods study. BMC Health Serv Res. 2021; 21(1): 1201. [DOI: 10.1186/s12913-021-07219-0]
26. Ogundeji Y, Clement F, Wellstead D, Farkas B, Manns B. Primary care physicians' perceptions of the role of alternative payment models in recruitment and retention in rural Alberta: A qualitative study. CMAJ Open. 2021; 9(3): E788-E94. [DOI: 10.9778/cmajo.20200202]
27. Bashar F, Islam R, Khan ShM, Hossain Sh, Sikder AAS, Yusuf SSh, et al. Making doctors stay: Rethinking doctor retention policy in a contracted-out primary healthcare setting in urban Bangladesh. PLoS ONE. 2022; 17(1): e0262358. [DOI: 10.1371/journal.pone.0262358]
28. Morken C, Bruksch-Meck K, Crouse B, Traxler K. Factors influencing rural physician retention following completion of a rural training track family medicine residency program. WMJ. 2018; 117(5): 208-10.
29. Asefzadeh S, Rafiei S, Ranjbar M, Kazemifar A, Akbari Sh. Influencing factors on physicians' retention in training hospitals of Qazvin University of Medical Sciences in 2017-2018. Evidence Based Health Policy, Management & Economics. 2020; 4(1): 23-31. [DOI: 10.18502/jebhpme.v4i1.2554]
30. Amiresmaili M, Jamebozorgi MH, Jamebozorgi AH, Arab-Zozani M. Retention of dental practitioners in rural health services in Iran: Experiences from Kerman province. Dental Research Journal. 2022; 19: 34.
31. Davari F, Sajadi, HS, Ehsani-Chimeh E, Alimohammadzade K. Incentive policies for the retention of physicians and nurses in deprived areas of the Islamic Republic of Iran. Health Information Management. 2020; 17(4): 159-66. [DOI: 10.22122/him.v17i4.4093]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |