Volume 6, Issue 1 (1-2022)
EBHPME 2022, 6(1): 41-51 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Gholizadeh M, Heydari S, Mir N, Taghipour H, Hatamzadeh N, Jalilian H. Evaluation of Self-Care and its Association with Quality of Life in Patients with Type 2 Diabetes. EBHPME 2022; 6 (1) :41-51
URL: http://jebhpme.ssu.ac.ir/article-1-358-en.html
URL: http://jebhpme.ssu.ac.ir/article-1-358-en.html
Masoumeh Gholizadeh 

 , Somayeh Heydari
, Somayeh Heydari 

 , Nazanin Mir
, Nazanin Mir 

 , Havjin Taghipour
, Havjin Taghipour 

 , Nasser Hatamzadeh
, Nasser Hatamzadeh 

 , Habib Jalilian *
, Habib Jalilian * 




 , Somayeh Heydari
, Somayeh Heydari 

 , Nazanin Mir
, Nazanin Mir 

 , Havjin Taghipour
, Havjin Taghipour 

 , Nasser Hatamzadeh
, Nasser Hatamzadeh 

 , Habib Jalilian *
, Habib Jalilian * 


Department of Health Services Management, School of Public Health, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran , jalilian.mg86@gmail.com
Full-Text [PDF 2266 kb]
(909 Downloads)
| Abstract (HTML) (2375 Views)
Full-Text: (676 Views)
Background: Diabetes is a chronic illness which requires continuous self-care. Appropriate self-care can reduce the risks of developing complications and improve the Quality of Life (QoL). This study aimed to examine self-care and its association with quality of life in patients with type 2 diabetes (T2DM) in East Azerbaijan, Iran, in 2018.
Methods: This was a cross-sectional study. The statistical population included all patients with type 2 diabetes in East Azerbaijan, in 2018. 310 patients were included using consecutive sampling. The summary of Diabetes Self-Care Activities Questionnaire (SDSCA) and the 12-Item Short Form Health Survey questionnaire (SF-12) were used for data collection. Data were analyzed using SPSS22. Descriptive statistics such as mean, Standard Deviation (SD), frequency, and percentage were applied to describe the characteristics of the respondents. The Spearman correlation, Mann Whitney U and Kruskal–Wallis tests were applied for statistical analysis.
Results: The mean scores of self-care and QoL were estimated to be 42.14 ± 61.63 and 53.25 ± 51.73, respectively. The highest mean of self-care and QoL was related to medications and social functioning which were 96.03 and 68.34. There was no correlation between the total mean score of self-care and QoL (P-value = 0.65). Moreover, a significant correlation was found between medication (insulin), exercise, blood-glucose testing and the total score of QoL (P-value < 0 .05).
Conclusion: The results indicated that self-care in patients with diabetes is poor, and the patients’ QoL is moderate. Therefore, it is suggested that managers of health centres take appropriate measures such as educational programs and executive interventions to enhance self-care in patients with diabetes. Moreover, to increase QoL, more attention should be paid to promote exercise and diet behaviours.
Key words: Type 2 diabetes mellitus, Self-care, Self-management, Quality of life
T2DM has a strong destructive influence on communities due to the severe comorbidities and complications of the disease (5). Diabetes care is complex and requires continuous medical care, glycemic control, and self-care measures to manage its complications (6). Self-care in diabetes is defined as an evolutionary process of the development of knowledge and awareness by learning to survive, concerning the complex nature of diabetes in a social context (7). Self-care behaviors in T2DM patients involve healthy eating, being active, self-monitoring, taking medications, reducing risks, etc. (8). Self-care is crucial to maintaining optimal glycaemic control and preventing complications (9), including microvascular and macrovascular complications. This can negatively affect Health-Related Quality of Life (HRQOL) (10,11) and have fatal consequences (12). The QoL of the patients with type 2 diabetes can be influenced by disease progression and response to medication therapy (13). T2DM has unfavorable effects on the HRQOL of the patients (13,14). Diabetes self-care activities are positively related to HRQOL for adhering patients (15), and those with low adherence to self-care activities (exercise and medication) have lower HRQOL (14).
Since most health care providers focus on medical outcomes only when assessing the efficacy of their interventions, assessing the QoL is crucial to achieve a better outcome and assess its effect on physical, emotional, social, and economic well-being (16). Studies regarding QoL can help evaluate a patient's psychological functioning, identify specific shortcomings, and the needs of patients at different stages of the disease, and compare the impact of various treatment regimens on a patient’s well-being and satisfaction (17). Such studies can also help clinicians predict the treatment response and survival time in certain contexts (18).
The impact of chronic disease on patients’ QoL is a concern for physicians and the patients themselves. This is particularly relevant in the case of diabetic patients (19). According to previous studies, the QoL for patients with diabetes is lower than that of healthy individuals (20).
Given the growing prevalence of diabetes and the importance of self-care in patients with diabetes, as well as the importance of assessing the QoL in chronic disease as the final outcome of disease management, this study aimed to examine the relationship between self-care and quality of life among patients with type 2 diabetes, in East Azerbaijan, Iran, in 2018.
Materials and Methods
Study design and participants
This was a cross-sectional study. The statistical population included all patients with type 2 diabetes in East Azerbaijan, in 2018.
Sampling and sample size
Given the number of people with diabetes in East Azerbaijan (331,500), the sample size was estimated to be 310 patients using Cochran's sample size formula (n = 𝑁𝑡2𝑝𝑞/𝑁𝑑2+𝑡2𝑝𝑞). In this study, at first, eight centers (5 urban health centers and 3 rural health centers) out of 84 centers were randomly selected. Next, all patients referring to these health centers over three months were included using the consecutive sampling. The questionnaire was distributed among participants referring to health centers. Participants who were able to read and write filled out the questionnaire, while the questions were read to the illiterate participants who responded accordingly.
Data collection tools
In this study, two questionnaires were used for data collection: 1) the Summary of Diabetes Self-Care Activities Questionnaire (SDSCA) and 2) the 12-Item Short Form Health Survey (SF-12). SDSCA questionnaire is the revised form of the "Diabetes Self-Care Activities Questionnaire” (DSCA), which was developed by Toobert
and Glasgow (1994) (21). This questionnaire consisted of 12 questions and 5 sub-scales: diet (4 items), exercise (2 items), blood-glucose testing (2 items), foot care (2 items) and medication (insulin) (2 item). Items were scored on a 7-point Likert scale with higher score reflecting better self-care. Cronbach's alpha of the self-care questionnaire was estimated at .86. The reliability and validity of the questionare has alreaddy been confirmed in the study of Poursharifi in Iran, in 2007 (22).
QoL was assessed using the SF-12 questionnaire. The SF-12 is one of the most widely used instruments for assessing self-reported health-related quality of life (HRQoL), which was developed from the Medical Outcomes Study (MOS) 36-item Short-Form Health Survey SF-36 (23). The questionnaire consisted of 12 questions with eight subscales: physical activity (2 items), physical role functioning (2 items), bodily pain (1 item), social functioning (1 items), emotional role functioning (2 items), vitality (1 items), mental health (2 items), and general health perceptions (1 item). Response categories for items vary from 2- to 6-point scales and raw scores for items rang from 1 to 6. Each subscale was analyzed in three different levels: favourable QoL (67-100), moderate QoL (33-66) and unfavourable QoL (0-32). Cronbach's alpha of the SF-12 questionnaire was estimated at 0.82. The reliability and validity of the questionare has alreaddy been confirmed in the study of Montazeri et al. (24) in Iran, in 2009. In order to better comprehend the scales of self-care and QoL, the score of all subscales was normalized according to the formula given below;
((the obtained score in subscale - the possible lowest subscale)/(the possible highest subscale - the possible lowest subscale)) × 100
Inclusion and exclusion criteria
Inclusion criteria were: Patients with type 2 diabetes who were 30 or above. Those who had physical and mental disabilities were excluded.
Data Analysis
Data were analyzed using SPSS22. Patients’ self-care and QoL were assessed through descriptive statistics (frequency, percet, mean and SD). Due to the non-normal distribution of data, the Spearman correlation was used to assess the correlation between self-care and QOL. Besides, Mann-Whitney and Kruskal-Wallis tests were used to examine the association between demographic variables and self-care and the QoL. The significance level for all statistical tests was set at P-values < 0.05 and <0.01.
This study was approved by the ethics committees of the Health Services Management Research Center, in Tabriz University of Medical Sciences.[reference number: IT. TBZMED REC.1396.974]. All participants were informed about the purpose of the study, their freedom to withdraw from the study at any time or answer any specific question, and assured of its confidentiality and anonymity.
Results
Demographic characteristics are shown in Table 1. A total of 310 patients with diabetes were included in the analysis, of whom 54.50 % were females and 45.50 % were males. The mean age of the patients was 59.79. 42.60 % of the patients were illiterate, and 63.50 % were unemployed. The majority of patients (88.70 %) were living in urban areas. The mean length of hospital stay and disease duration was estimated at 1.20 and 6.66 days, respectively.
The total score of QoL and self-care were significantly associated with education, job status, habitation status, hospitalization history, and complications (P-value < 0.05). The total scores of QoL and self-care were higher in patients who
had higher education, were living in urban areas, and had no history of hospitalization and complications. Besides, a significant association was found between the total score of QoL and income status (Table 1).
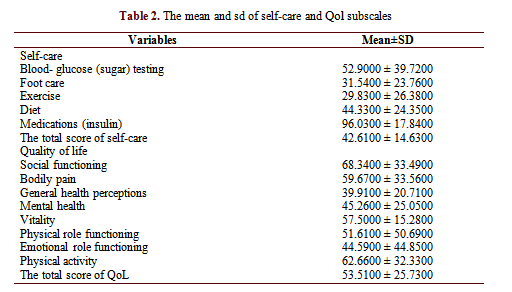
The descriptive results of self-care and QoL are shown in Table 2. The highest and lowest mean of self-care subscales were related to medication (insulin) and exercise, which were 96.03 and 29.83, respectively. The highest and lowest QoL subscales were related to social functioning and general health perceptions, which were 68.34 and 39.91.
According to the Spearman correlation coefficient test in Table 3, the variables of age, disease duration and number of hospitalizations were negatively correlated with all subscales of QoL (P-value < 0.05). The blood-glucose testing was positively correlated with the number of hospitalizations, and diet was positively correlated with disease duration. There was a significant negative correlation between exercise and all variables of age, disease duration and number of hospitalizations. Also, foot care was positively related to age and the number of hospitalizations.
The total score of QoL was not significantly correlated with the total self-care score (P-value = 0.65). The exercise subscale had a significant positive correlation with all QoL subscales, and blood-glucose testing was negatively correlated with QoL subscales. There was a negative correlation between the medication (insulin) and general health perceptions, physical functioning, physical role functioning, social functioning, and QoL's total score. Furthermore, a positive correlation was found between diet and vitality as well as mental health. The total self-care score was positively correlated with mental health (Table 4).
1Mann Whitney U Test for two independent samples
2Kruskal–Wallis test for more than two independent samples
* Correlation is significant at the 0.05 level (2-tailed)
**Correlation is significant at the 0.01 level (2-tailed)
**Correlation is significant at the 0.01 level (2-tailed)
*Spearman correlation for correlation between two variables
* Correlation is significant at 0.05 level (2-tailed)
**Correlation is significant at the 0.01 level (2-tailed)
Discussion
This study was designed to examine self-care and its relationship with quality of life in patients with type 2 diabetes. The total score of self-care was low (42.61 of 100). The highest scores of self-care were related to medication (insulin) and blood glucose (sugar) testing, and the lowest scores were related to exercise, foot care, and diet. It seems that patients with type 2 diabetes paid more attention to blood glucose testing and medication compared with exercise, diet and foot care. The results were in line with the results of Ausili et al. (25) in Italy, which found that self-care regarding exercise and foot care was less than diet and blood glucose testing. Since poor adherence to exercise and foot care, unlike insulin injection, does not present its negative effect immediately, patients with diabetes pay little attention to adherence to exercise and diet. Adherence to exercise in T2DM is specified by complex physical, psychological and social variables (26), and many of these variables can be taken into account barriers to physical activity (27). Service providers, therefore, should inform patients with diabetes of the importance of diet adherence and physical activity. It has been shown that exercise is the most important determinant of positive clinical outcomes in patients with T2DM (25). Notably, since adherence to a regular diet, physical activity, and foot care generally requires more time than insulin injection and blood glucose testing, it seems that patients' families can help them with adherence to a healthy diet and regular physical activity, and provide them with necessary social supports.
In this study, the total mean score of QoL was moderate (53.51 of 100). The highest score of the QoL subscales was related to social functioning, followed by physical activity and bodily pain. General health perceptions, emotional role functioning and mental health, had the lowest scores, respectively. It was revealed that the negative psychological effects of diabetes were higher than its physical and social effects. Delahanty et al. (28) demonstrated that psychological factors such as diabetes-related emotional distress are related to less adherence to diet, exercise, frequent blood glucose testing and medication regimens. It has been shown that people with diabetes suffer from a higher burden of psychosocial problems and disorders (29). Therefore, the presence of a psychologist in the diabetes care team can improve diabetic patients’ QoL. Additionally, psychological intervention in patients with type 2 diabetes who are experiencing psychological problems can improve psychological health, quality of life, and health outcomes (29).
In this study, those with higher education and better job status had better QoL and self-care, meaning that higher socioeconomic status is an influential factor in improving QoL and self-care in patients with Type 2 diabetes. Another study in Iran (30) revealed that self-care behavior was positively correlated with employment and education. Moreover, patients living in urban areas had better QoL, while those living in rural areas had a better self-care status. It may be due to the fact that rural patients mostly refer to the primary care centers, and these centers concentrate more on primary care, preventive measures, consultant services and health education, while advanced therapeutic centers in urban areas offer more clinical treatment.
Further, those without a history of hospitalization had better QoL, while those with a history of hospitalization had better adherence to self-care measures. This may be because patients who had a history of hospitalization were in a severe condition. The severity of the disease causes patients to adhere more to self-care measures. The diet and self-care subscales were significantly correlated with vitality and mental health, which indicated patients with better adherence to diet measures would have better QoL. A study suggested that better self-care was associated with better metabolic and lipid control, better Hemoglobin A1c (HbA1c) control and better
QoL (31).
Moreover, exercise was significantly correlated with all subscales of QoL. This indicated that better adherence to exercise improves all subscales of patients' QoL. On the other hand, it is possible that better QoL may affect patients' ability to adhere to an exercise program. Ilhan et al. (32) conducted a study to examine the relationship between health literacy and diabetes self-care in individuals with T2DM and discovered that education and exercise status were significantly related to diabetes self-care. A study in Malaysia showed that exercise was a crucial part of diabetes management since it improved HbA1c levels, reduced weight and decreased the occurrence of further complications (33).
Conversely, blood glucose monitoring and medication (insulin) were negatively correlated with QoL. However, given that this was a correlational study, the causal effect could not be clarified, and this can be a reciprocal interaction. Those with better QoL were more likely to focus on a healthy diet and exercise. In contrast, those with lower QoL were more likely to focus on blood glucose monitoring and medication. It seems that adherence to exercise and diet is more likely to improve patients' QoL than blood-glucose monitoring and medication. Better self-care can lead to better QoL, and lower QoL can be a barrier to adherence to self-care. Baraz et al. (34) showed that a self-care education program resulted in a significant increase in general health, physical role, physical functioning, social functioning and bodily pain.
In this study, patients with no complications had better QoL and self-care. Better adherence to self-care measures can result in a lower incidence of diabetes complications. Shea et al. (35) found that the highest level of physical activity was reported in respondents with no comorbidity, while the lowest was in patients with both concordant and discordant comorbidity.
The results of this study indicated that with increasing age and duration of the disease, patients’ QoL decreases. Also, it was found that with increasing age, patients’ self-care measures such as foot care, physical activity and exercise decrease, suggesting that an increase in age may be associated with a decline in physical functioning, affecting patients’ self-care. It seems that older people need more advice, education and support to better adhere to self-care measures. Younger family members should take care of older people and provide them with appropriate information about foot care. A previous study found that family and social support are important aspects of adherence to diabetes management, and also positive dimensions of family functioning, including family guidance and control over the management of diabetes, are related to the increase in adherence behaviors (36).
The study's limitation can be related to the cross-sectional design of the research, which does not make it possible to evaluate the causal effect of self-care on QoL. Hence, it is necessary to conduct controlled experimental studies focusing on patients with the same disease severity and controlling other factors like a sociodemographic variable.
Conclusion
This study suggested that self-care in patients with diabetes is poor, and the patients’ QoL is moderate. Patients with a more severe condition and poor QoL showed better adherence to the blood-glucose testing and medication, while those with better QoL had better adherence to the diet and exercise behaviors. It is suggested that managers of health centres take appropriate measures such as educational programs and executive interventions to enhance self-care in patients with diabetes. Moreover, to increase QoL, more attention should be paid to promoting exercise and diet behaviours.
Considering the implementation of the Iran- Package of Essential Non-communicable Disease )IRAPEN(and its emphasis on preventive measures and active care, and its focus on self-care in diabetes management, it can be concluded that the health centers' performance in this regard has generally not been satisfactory. Therefore, due to the poor self-care status in patients with diabetes, it is necessary for the managers of health centers to pursue the educational programs and executive interventions related to self-care in patients with diabetes, especially in the subscales of physical activity and diet more seriously. These centers need to attract other non-governmental organizations such as the East Azerbaijan Diabetes Association and social media and involve patients' families in the process.
Acknowledgements
The authors gratefully acknowledge the financial support provided by the Tabriz Health service management research centre, at Tabriz University of Medical Sciences. Also, we thank the staff of all selected health centers and patients for their kind support and participation in this study.
Conflict of interests
The authors declared no conflict of interests.
Authors’ contributions
Jalilian H and Gholizadeh M designed research; Jalilian H, Heydari S, Mir N, Taghipour H, and Hatamzadeh N conducted research; Jalilian H analyzed data; and Jalilian H and Heydari S wrote the paper. Jalilian H had had primary responsibility for the final content. All authors read and approved the final manuscript.
Funding
This study was financed by the Tabriz Health Service Management Research Centre, Tabriz University of Medical Sciences.
Methods: This was a cross-sectional study. The statistical population included all patients with type 2 diabetes in East Azerbaijan, in 2018. 310 patients were included using consecutive sampling. The summary of Diabetes Self-Care Activities Questionnaire (SDSCA) and the 12-Item Short Form Health Survey questionnaire (SF-12) were used for data collection. Data were analyzed using SPSS22. Descriptive statistics such as mean, Standard Deviation (SD), frequency, and percentage were applied to describe the characteristics of the respondents. The Spearman correlation, Mann Whitney U and Kruskal–Wallis tests were applied for statistical analysis.
Results: The mean scores of self-care and QoL were estimated to be 42.14 ± 61.63 and 53.25 ± 51.73, respectively. The highest mean of self-care and QoL was related to medications and social functioning which were 96.03 and 68.34. There was no correlation between the total mean score of self-care and QoL (P-value = 0.65). Moreover, a significant correlation was found between medication (insulin), exercise, blood-glucose testing and the total score of QoL (P-value < 0 .05).
Conclusion: The results indicated that self-care in patients with diabetes is poor, and the patients’ QoL is moderate. Therefore, it is suggested that managers of health centres take appropriate measures such as educational programs and executive interventions to enhance self-care in patients with diabetes. Moreover, to increase QoL, more attention should be paid to promote exercise and diet behaviours.
Key words: Type 2 diabetes mellitus, Self-care, Self-management, Quality of life
Introduction
Type 2 Diabetes Mellitus (T2DM) makes up more than 90 % of all diabetic patients, and its prevalence is increasing worldwide (1). In 2019, approximately 463 million adults (20-79) had diabetes, but it is predicted that by 2045 this figure would rise to 700 million (2). The proportion of people with type 2 diabetes is increasing in most countries. 79 % of the adults with diabetes live in LOW-and Middle-Income Countries (LMICs) (2). 80 % of people with diabetes live in LMICs, and the prevalence rate of diabetes is accelerating in poorer communities (3). As one of the developing countries in the Middle East, Iran is facing an increase in the prevalence of the disease. In Iran, in 2020, the total cases of diabetes and the prevalence rate of diabetes in adults were estimated to be 5,387,200 and 9.40 %, respectively (4).T2DM has a strong destructive influence on communities due to the severe comorbidities and complications of the disease (5). Diabetes care is complex and requires continuous medical care, glycemic control, and self-care measures to manage its complications (6). Self-care in diabetes is defined as an evolutionary process of the development of knowledge and awareness by learning to survive, concerning the complex nature of diabetes in a social context (7). Self-care behaviors in T2DM patients involve healthy eating, being active, self-monitoring, taking medications, reducing risks, etc. (8). Self-care is crucial to maintaining optimal glycaemic control and preventing complications (9), including microvascular and macrovascular complications. This can negatively affect Health-Related Quality of Life (HRQOL) (10,11) and have fatal consequences (12). The QoL of the patients with type 2 diabetes can be influenced by disease progression and response to medication therapy (13). T2DM has unfavorable effects on the HRQOL of the patients (13,14). Diabetes self-care activities are positively related to HRQOL for adhering patients (15), and those with low adherence to self-care activities (exercise and medication) have lower HRQOL (14).
Since most health care providers focus on medical outcomes only when assessing the efficacy of their interventions, assessing the QoL is crucial to achieve a better outcome and assess its effect on physical, emotional, social, and economic well-being (16). Studies regarding QoL can help evaluate a patient's psychological functioning, identify specific shortcomings, and the needs of patients at different stages of the disease, and compare the impact of various treatment regimens on a patient’s well-being and satisfaction (17). Such studies can also help clinicians predict the treatment response and survival time in certain contexts (18).
The impact of chronic disease on patients’ QoL is a concern for physicians and the patients themselves. This is particularly relevant in the case of diabetic patients (19). According to previous studies, the QoL for patients with diabetes is lower than that of healthy individuals (20).
Given the growing prevalence of diabetes and the importance of self-care in patients with diabetes, as well as the importance of assessing the QoL in chronic disease as the final outcome of disease management, this study aimed to examine the relationship between self-care and quality of life among patients with type 2 diabetes, in East Azerbaijan, Iran, in 2018.
Materials and Methods
Study design and participants
This was a cross-sectional study. The statistical population included all patients with type 2 diabetes in East Azerbaijan, in 2018.
Sampling and sample size
Given the number of people with diabetes in East Azerbaijan (331,500), the sample size was estimated to be 310 patients using Cochran's sample size formula (n = 𝑁𝑡2𝑝𝑞/𝑁𝑑2+𝑡2𝑝𝑞). In this study, at first, eight centers (5 urban health centers and 3 rural health centers) out of 84 centers were randomly selected. Next, all patients referring to these health centers over three months were included using the consecutive sampling. The questionnaire was distributed among participants referring to health centers. Participants who were able to read and write filled out the questionnaire, while the questions were read to the illiterate participants who responded accordingly.
Data collection tools
In this study, two questionnaires were used for data collection: 1) the Summary of Diabetes Self-Care Activities Questionnaire (SDSCA) and 2) the 12-Item Short Form Health Survey (SF-12). SDSCA questionnaire is the revised form of the "Diabetes Self-Care Activities Questionnaire” (DSCA), which was developed by Toobert
and Glasgow (1994) (21). This questionnaire consisted of 12 questions and 5 sub-scales: diet (4 items), exercise (2 items), blood-glucose testing (2 items), foot care (2 items) and medication (insulin) (2 item). Items were scored on a 7-point Likert scale with higher score reflecting better self-care. Cronbach's alpha of the self-care questionnaire was estimated at .86. The reliability and validity of the questionare has alreaddy been confirmed in the study of Poursharifi in Iran, in 2007 (22).
QoL was assessed using the SF-12 questionnaire. The SF-12 is one of the most widely used instruments for assessing self-reported health-related quality of life (HRQoL), which was developed from the Medical Outcomes Study (MOS) 36-item Short-Form Health Survey SF-36 (23). The questionnaire consisted of 12 questions with eight subscales: physical activity (2 items), physical role functioning (2 items), bodily pain (1 item), social functioning (1 items), emotional role functioning (2 items), vitality (1 items), mental health (2 items), and general health perceptions (1 item). Response categories for items vary from 2- to 6-point scales and raw scores for items rang from 1 to 6. Each subscale was analyzed in three different levels: favourable QoL (67-100), moderate QoL (33-66) and unfavourable QoL (0-32). Cronbach's alpha of the SF-12 questionnaire was estimated at 0.82. The reliability and validity of the questionare has alreaddy been confirmed in the study of Montazeri et al. (24) in Iran, in 2009. In order to better comprehend the scales of self-care and QoL, the score of all subscales was normalized according to the formula given below;
((the obtained score in subscale - the possible lowest subscale)/(the possible highest subscale - the possible lowest subscale)) × 100
Inclusion and exclusion criteria
Inclusion criteria were: Patients with type 2 diabetes who were 30 or above. Those who had physical and mental disabilities were excluded.
Data Analysis
Data were analyzed using SPSS22. Patients’ self-care and QoL were assessed through descriptive statistics (frequency, percet, mean and SD). Due to the non-normal distribution of data, the Spearman correlation was used to assess the correlation between self-care and QOL. Besides, Mann-Whitney and Kruskal-Wallis tests were used to examine the association between demographic variables and self-care and the QoL. The significance level for all statistical tests was set at P-values < 0.05 and <0.01.
This study was approved by the ethics committees of the Health Services Management Research Center, in Tabriz University of Medical Sciences.[reference number: IT. TBZMED REC.1396.974]. All participants were informed about the purpose of the study, their freedom to withdraw from the study at any time or answer any specific question, and assured of its confidentiality and anonymity.
Results
Demographic characteristics are shown in Table 1. A total of 310 patients with diabetes were included in the analysis, of whom 54.50 % were females and 45.50 % were males. The mean age of the patients was 59.79. 42.60 % of the patients were illiterate, and 63.50 % were unemployed. The majority of patients (88.70 %) were living in urban areas. The mean length of hospital stay and disease duration was estimated at 1.20 and 6.66 days, respectively.
The total score of QoL and self-care were significantly associated with education, job status, habitation status, hospitalization history, and complications (P-value < 0.05). The total scores of QoL and self-care were higher in patients who
had higher education, were living in urban areas, and had no history of hospitalization and complications. Besides, a significant association was found between the total score of QoL and income status (Table 1).
The descriptive results of self-care and QoL are shown in Table 2. The highest and lowest mean of self-care subscales were related to medication (insulin) and exercise, which were 96.03 and 29.83, respectively. The highest and lowest QoL subscales were related to social functioning and general health perceptions, which were 68.34 and 39.91.
According to the Spearman correlation coefficient test in Table 3, the variables of age, disease duration and number of hospitalizations were negatively correlated with all subscales of QoL (P-value < 0.05). The blood-glucose testing was positively correlated with the number of hospitalizations, and diet was positively correlated with disease duration. There was a significant negative correlation between exercise and all variables of age, disease duration and number of hospitalizations. Also, foot care was positively related to age and the number of hospitalizations.
The total score of QoL was not significantly correlated with the total self-care score (P-value = 0.65). The exercise subscale had a significant positive correlation with all QoL subscales, and blood-glucose testing was negatively correlated with QoL subscales. There was a negative correlation between the medication (insulin) and general health perceptions, physical functioning, physical role functioning, social functioning, and QoL's total score. Furthermore, a positive correlation was found between diet and vitality as well as mental health. The total self-care score was positively correlated with mental health (Table 4).
Table 1. The mean and sd of self-care and Qol divided by the variables
| Variables | Modes | Frequency (percent) | The total score of QoL | The total score of self-care | ||
| Mean±SD | P | Mean ±SD | P | |||
| Gender1 | Male | 144 (45.5000) | 52.7100 ± 26.3300 | 0.7000 | 42.8500 ± 15.2100 | 0.9600 |
| Female | 166 (54.5000) | 54.2000 ± 25.2700 | 42.4000 ± 14.1500 | |||
| Marital status | Married | 287 (92.6000) | 48.6000 ± 29.5500 | 0.3400 | 44.6700 ± 19.2700 | 0.9600 |
| Single | 23 (7.4000) | 53.9100 ± 25.4200 | 42.4400 ± 14.2300 | |||
| Education status2 | Illiterate | 132 (42.6000) | 43.8700 ± 24.5700 | < 0.0001** | 40.0800 ± 14.8600 | < 0.0001** |
| Elementary | 80 (25.8000) | 54.0700 ± 23.2100 | 41.1400 ± 12.7000 | |||
| Middle | 36 (11.6000) | 60.0900 ± 25.6200 | 43.2500 ± 16.1900 | |||
| Diploma | 43 (13.9000) | 68.2100 ± 22.0600 | 47.6700 ± 12.4400 | |||
| University | 19 (6.1000) | 71.9000 ± 23.3900 | 53.6500 ± 15.6100 | |||
| Job status | Unemployed | 197 (63.5000) | 49.0900 ± 25.0100 | < 0.0001** | 40.5600 ± 12.7200 | < 0.0001** |
| Worker | 47 (15.2000) | 63.9700 ± 26.6800 | 37.9200 ± 14.8600 | |||
| Employee | 15 (4.8000) | 66.9500 ± 24.7300 | 59.5200 ± 15.0900 | |||
| Retired | 51 (16.5000) | 55.1300 ± 24.8700 | 45.3500 ± 16.6800 | |||
| Income status | Less than livelihood | 109 (35.2000) | 45.3400 ± 23.5700 | < 0.0001** | 43.8400 ± 15.0600 | 0.2900 |
| Equal to livelihood | 164 (52.9000) | 56.3100 ± 26.4200 | 42.6400 ± 14.9900 | |||
| More than livelihood | 37 (11.9000) | 65.0100 ± 21.9500 | 38.8500 ± 11.0300 | |||
| Health insurance status | Yes | 273 (88.1000) | 54.1400 ± 25.5800 | 0.7300 | 43.06 00± 14.9200 | 0.1200 |
| No | 37 (11.9000) | 48.8600 ± 26.6900 | 39.2900 ± 12.0100 | |||
| Habitation status | Living in urban areas | 275 (88.7000) | 55.2500 ± 25.3300 | < 0.0010** | 41.88 00± 14.3800 | 0.0100* |
| Living in rural areas | 35 (11.3000) | 39.9300 ± 25.1200 | 48.3600 ± 15.5400 | |||
| The history of hospitalization during the past year | No | 184 (59.4000) | 63.8600 ± 24.8000 | < 0.0001** | 40.1100 ± 13.5300 | < 0.0001** |
| Yes | 126 (40.6000) | 38.3600 ± 18.6300 | 46.2600 ± 15.4500 | |||
| Complication | Yes | 100 (32.3000) | 44.1600 ± 24.9700 | < 0.0010** | 38.5600 ± 12.6500 | < 0.0010** |
| No | 210 (67.7000) | 58.0000 ± 24.1900 | 44.5400 ± 15.1400 | |||
2Kruskal–Wallis test for more than two independent samples
* Correlation is significant at the 0.05 level (2-tailed)
**Correlation is significant at the 0.01 level (2-tailed)
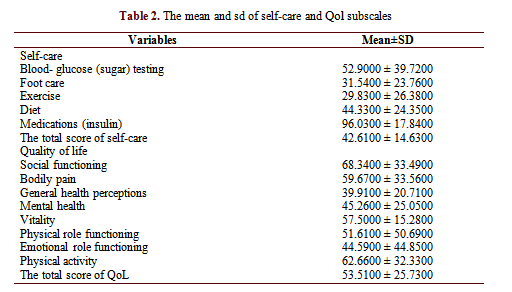
Table 3. Correlation between self-care and Qol and age, disease duration, and number of hospitalization
| Variables | Age | Disease duration | Number of hospitalization |
| Blood- glucose testing | 0.0100 | 0.0200 | 0.4300** |
| 0.7600 | 0.7200 | < 0.0001 | |
| Diet | - 0.0400 | 0.1400** | 0.0600 |
| 0.4200 | 0.0000 | 0.2300 | |
| Exercise | - 0.4000** | - 0.4200** | - 0.5600** |
| < 0.0001 | <0.0001 | < 0.0001 | |
| Foot care | - 0.1200* | - 0.0200 | 0.1800** |
| 0.0300 | 0.6200 | 0.0000 | |
| Medications (insulin) | 0.1000 | 0.0700 | 0.1000 |
| 0.0500 | 0.2100 | 0.0700 | |
| The total score of self-care | - 0.1700** | - 0.0100 | 0.2000** |
| 0.0000 | 0.7700 | < 0.0001 | |
| General health perceptions | - 0.4000** | - 0.2900** | - 0.4700** |
| < 0.0001 | < 0.0001 | < 0.0001 | |
| Bodily pain | - 0.3100** | - 0.2800** | - 0.4800** |
| < 0.0001 | < .0001 | <0.0001 | |
| Social functioning | - 0.3800** | - 0.2800** | - 0.5300** |
| < 0.0001 | < .0001 | < 0.0001 | |
| Mental health | - 0.4900** | - 0.3500** | - 0.6100** |
| < 0.0001 | < .0001 | < 0.0001 | |
| Vitality | - 0.4700** | - 0.4000** | - 0.6000** |
| < 0.0001 | < 0.0001 | < 0.0001 | |
| Physical role functioning | - 0.3600** | - 0.3400** | - 0.5500** |
| < 0.0001 | < 0.0001 | < 0.0001 | |
| Emotional role functioning | - 0.3600** | - 0.2900** | - 0.3600** |
| < 0.0001 | < 0.0001 | < 0.0001 | |
| Physical activity | - 0.3600** | - 0.3400** | - 0.3800** |
| < 0.0001 | < 0.0001 | < 0.0001 | |
| The total score of QOL | - 0.4700** | - 0.3900** | - 0.6200** |
| < 0.0001 | < 0.0001 | < 0.0001 |
*Spearman correlation for correlation between two variables
Table 4. Correlation between self-care and Qol
| Variables | Foot care | Diet | Exercise | Blood-glucose testing | Medications (insulin) |
Total score of self-care |
| General health perceptions | - 0.0900 | 0.1200 | 0.500** | - 0.270** | - 0.130* | - 0.0010 |
| 0.1000 | 0.0200 | < 0.001 | < 0.001 | 0.010 | 0.8700 | |
| Physical functioning | - 0.0100 | 0.0700 | 0.700** | - 0.480** | - 0.120* | - 0.0100 |
| 0.8600 | 0.2100 | < 0.001 | < 0.001 | 0.030 | 0.7700 | |
| Physical role functioning | - 0.0600 | - 0.0000 | 0.650** | - 0.490** | - 0.130* | - 0.0800 |
| 0.2300 | 0.9300 | < 0.001 | < 0.001 | 0.010 | 0.1500 | |
| Emotional role functioning | - 0.04 | 0.0000 | 0.4900** | -0.6500** | - 0.0100 | - 0.7900 |
| 0.43 | 0.8300 | < 0.0010 | < 0.0010 | 0.8200 | 0.1600 | |
| Social role functioning | - 0.09 | 0.0700 | 0.5400** | - 0.4000** | - 0.1700** | - 0.0800 |
| 0.10 | 0.2100 | < 0.0010 | < 0.0010 | < 0.0010 | 0.1500 | |
| Bodily pain | - 0.09 | 0.0300 | 0.4900** | - 0.4000** | -0.0700 | - 0.0900 |
| 0.08 | 0.5700 | < 0.0010 | < 0.0010 | 0.2100 | 0.0800 | |
| Vitality | 0.06 | 0.1900** | 0.3500** | - 0.1100** | - 0.0400 | 0.1400 |
| 0.29 | < 0.0010 | < 0.0010 | < 0.0010 | 0.4200 | 0.0100 | |
| Mental health | 0.07 | 0.1600** | 0.4200** | - 0.0900** | - 0.0700 | 0.1600 |
| 0.02 | < 0.0010 | < 0.0010 | < 0.0010 | 0.1800 | < 0.0010 | |
| Total score of quality of life | - 0.03 | 0.0800 | 0.9100** | - 0.4700** | - 0.1100* | - 0.0200 |
| 0.50 | 0.1400 | < 0.0010 | < 0.0010 | 0.0300 | 0.6500 |
**Correlation is significant at the 0.01 level (2-tailed)
Discussion
This study was designed to examine self-care and its relationship with quality of life in patients with type 2 diabetes. The total score of self-care was low (42.61 of 100). The highest scores of self-care were related to medication (insulin) and blood glucose (sugar) testing, and the lowest scores were related to exercise, foot care, and diet. It seems that patients with type 2 diabetes paid more attention to blood glucose testing and medication compared with exercise, diet and foot care. The results were in line with the results of Ausili et al. (25) in Italy, which found that self-care regarding exercise and foot care was less than diet and blood glucose testing. Since poor adherence to exercise and foot care, unlike insulin injection, does not present its negative effect immediately, patients with diabetes pay little attention to adherence to exercise and diet. Adherence to exercise in T2DM is specified by complex physical, psychological and social variables (26), and many of these variables can be taken into account barriers to physical activity (27). Service providers, therefore, should inform patients with diabetes of the importance of diet adherence and physical activity. It has been shown that exercise is the most important determinant of positive clinical outcomes in patients with T2DM (25). Notably, since adherence to a regular diet, physical activity, and foot care generally requires more time than insulin injection and blood glucose testing, it seems that patients' families can help them with adherence to a healthy diet and regular physical activity, and provide them with necessary social supports.
In this study, the total mean score of QoL was moderate (53.51 of 100). The highest score of the QoL subscales was related to social functioning, followed by physical activity and bodily pain. General health perceptions, emotional role functioning and mental health, had the lowest scores, respectively. It was revealed that the negative psychological effects of diabetes were higher than its physical and social effects. Delahanty et al. (28) demonstrated that psychological factors such as diabetes-related emotional distress are related to less adherence to diet, exercise, frequent blood glucose testing and medication regimens. It has been shown that people with diabetes suffer from a higher burden of psychosocial problems and disorders (29). Therefore, the presence of a psychologist in the diabetes care team can improve diabetic patients’ QoL. Additionally, psychological intervention in patients with type 2 diabetes who are experiencing psychological problems can improve psychological health, quality of life, and health outcomes (29).
In this study, those with higher education and better job status had better QoL and self-care, meaning that higher socioeconomic status is an influential factor in improving QoL and self-care in patients with Type 2 diabetes. Another study in Iran (30) revealed that self-care behavior was positively correlated with employment and education. Moreover, patients living in urban areas had better QoL, while those living in rural areas had a better self-care status. It may be due to the fact that rural patients mostly refer to the primary care centers, and these centers concentrate more on primary care, preventive measures, consultant services and health education, while advanced therapeutic centers in urban areas offer more clinical treatment.
Further, those without a history of hospitalization had better QoL, while those with a history of hospitalization had better adherence to self-care measures. This may be because patients who had a history of hospitalization were in a severe condition. The severity of the disease causes patients to adhere more to self-care measures. The diet and self-care subscales were significantly correlated with vitality and mental health, which indicated patients with better adherence to diet measures would have better QoL. A study suggested that better self-care was associated with better metabolic and lipid control, better Hemoglobin A1c (HbA1c) control and better
QoL (31).
Moreover, exercise was significantly correlated with all subscales of QoL. This indicated that better adherence to exercise improves all subscales of patients' QoL. On the other hand, it is possible that better QoL may affect patients' ability to adhere to an exercise program. Ilhan et al. (32) conducted a study to examine the relationship between health literacy and diabetes self-care in individuals with T2DM and discovered that education and exercise status were significantly related to diabetes self-care. A study in Malaysia showed that exercise was a crucial part of diabetes management since it improved HbA1c levels, reduced weight and decreased the occurrence of further complications (33).
Conversely, blood glucose monitoring and medication (insulin) were negatively correlated with QoL. However, given that this was a correlational study, the causal effect could not be clarified, and this can be a reciprocal interaction. Those with better QoL were more likely to focus on a healthy diet and exercise. In contrast, those with lower QoL were more likely to focus on blood glucose monitoring and medication. It seems that adherence to exercise and diet is more likely to improve patients' QoL than blood-glucose monitoring and medication. Better self-care can lead to better QoL, and lower QoL can be a barrier to adherence to self-care. Baraz et al. (34) showed that a self-care education program resulted in a significant increase in general health, physical role, physical functioning, social functioning and bodily pain.
In this study, patients with no complications had better QoL and self-care. Better adherence to self-care measures can result in a lower incidence of diabetes complications. Shea et al. (35) found that the highest level of physical activity was reported in respondents with no comorbidity, while the lowest was in patients with both concordant and discordant comorbidity.
The results of this study indicated that with increasing age and duration of the disease, patients’ QoL decreases. Also, it was found that with increasing age, patients’ self-care measures such as foot care, physical activity and exercise decrease, suggesting that an increase in age may be associated with a decline in physical functioning, affecting patients’ self-care. It seems that older people need more advice, education and support to better adhere to self-care measures. Younger family members should take care of older people and provide them with appropriate information about foot care. A previous study found that family and social support are important aspects of adherence to diabetes management, and also positive dimensions of family functioning, including family guidance and control over the management of diabetes, are related to the increase in adherence behaviors (36).
The study's limitation can be related to the cross-sectional design of the research, which does not make it possible to evaluate the causal effect of self-care on QoL. Hence, it is necessary to conduct controlled experimental studies focusing on patients with the same disease severity and controlling other factors like a sociodemographic variable.
Conclusion
This study suggested that self-care in patients with diabetes is poor, and the patients’ QoL is moderate. Patients with a more severe condition and poor QoL showed better adherence to the blood-glucose testing and medication, while those with better QoL had better adherence to the diet and exercise behaviors. It is suggested that managers of health centres take appropriate measures such as educational programs and executive interventions to enhance self-care in patients with diabetes. Moreover, to increase QoL, more attention should be paid to promoting exercise and diet behaviours.
Considering the implementation of the Iran- Package of Essential Non-communicable Disease )IRAPEN(and its emphasis on preventive measures and active care, and its focus on self-care in diabetes management, it can be concluded that the health centers' performance in this regard has generally not been satisfactory. Therefore, due to the poor self-care status in patients with diabetes, it is necessary for the managers of health centers to pursue the educational programs and executive interventions related to self-care in patients with diabetes, especially in the subscales of physical activity and diet more seriously. These centers need to attract other non-governmental organizations such as the East Azerbaijan Diabetes Association and social media and involve patients' families in the process.
Acknowledgements
The authors gratefully acknowledge the financial support provided by the Tabriz Health service management research centre, at Tabriz University of Medical Sciences. Also, we thank the staff of all selected health centers and patients for their kind support and participation in this study.
Conflict of interests
The authors declared no conflict of interests.
Authors’ contributions
Jalilian H and Gholizadeh M designed research; Jalilian H, Heydari S, Mir N, Taghipour H, and Hatamzadeh N conducted research; Jalilian H analyzed data; and Jalilian H and Heydari S wrote the paper. Jalilian H had had primary responsibility for the final content. All authors read and approved the final manuscript.
Funding
This study was financed by the Tabriz Health Service Management Research Centre, Tabriz University of Medical Sciences.
Type of Study: Original article |
Subject:
Healt care Management
Received: 2021/09/6 | Accepted: 2022/01/30 | Published: 2022/03/29
Received: 2021/09/6 | Accepted: 2022/01/30 | Published: 2022/03/29
References
1. Caluyong MB, Zambrana AF, Romanow HC, Nathan HJ, Nahas R, Poulin PA. The relationship between mindfulness, depression, diabetes self-care, and health-related quality of life in patients with type 2 diabetes. Mindfulness. 2015; 6(6): 1313-21. [DOI:10.1007/s12671-015-0401-z]
2. (IDF) TIDF. Diabetes facts & figures. Available from URL: https://idforg/aboutdiabetes/what-is-diabetes/facts-figureshtml. Latest Access: September 21, 2021.
3. Dunachie S, Chamnan P. The double burden of diabetes and global infection in low and middle-income countries. Transactions of The Royal Society of Tropical Medicine and Hygiene. 2019; 113(2): 56-64. [DOI:10.1093/trstmh/try124try124]
4. (IDF) TIDF. Diabetes facts & figures. MENA Members. Available from URL: https://idforg/ our-network/regions-members/middle-east-and-north-africa/ members/35-iranhtml. Latest Access: January 11, 2020.
5. Handelsman Y, Bloomgarden ZT, Grunberger G, Umpierrez G, Zimmerman RS, Bailey TS, et al. American association of clinical endocrinologists and American college of endocrinology-clinical practice guidelines for developing a Diabetes mellitus comprehensive care plan-2015. Endocrine Practice. 2015; 21(1): 1-87. [DOI:10.4158/EP15672.GL]
6. Association AD. Standards of medical care in diabetes. Diabetes care. 2005; 28(suppl 1): s4-s36. [DOI:10.2337/diacare.28.suppl_1.S4]
7. Shrivastava SR, Shrivastava PS, Ramasamy J. Role of self-care in management of diabetes mellitus. Journal of Diabetes & Metabolic Disorders. 2013; 12 (1): 1-5. [DOI:10.1186/2251-6581-12-14]
8. Powers MA, Bardsley J, Cypress M, Duker P, Funnell MM, Fischl AH, et al. Diabetes self-management education and support in type 2 Diabetes: A joint position statement of the American diabetes association, the American association of diabetes educators, and the academy of nutrition and dietetics. Clinical Diabetes. 2016; 34(2): 70-80. [DOI:10.2337/diaclin.34.2.70]
9. Funnell MM, Brown TL, Childs BP, Haas LB, Hosey GM, Jensen B, et al. National standards for Diabetes self-management education. Diabetes Care. 2009; 32(1): S87-S94. [DOI:10.2337/dc09-S087]
10. Ahola AJ, Saraheimo M, Forsblom C, Hietala K, Sintonen H, Groop P-H, et al. Health-related quality of life in patients with type 1diabetes-association with diabetic complications (the FinnDiane study). Nephrology Dialysis Transplantation. 2010; 25(6): 1903-8. [DOI:10.1093/ndt/gfp709]
11. Solli O, Stavem K, Kristiansen IS. Health-related quality of life in diabetes: The associations of complications with EQ-5D scores. Health and Quality of Life Outcomes. 2010; 8(1): 18. [DOI:10.1186/1477-7525-8-18]
12. Clarke W, Deeb LC, Jameson P, Kaufman F, Klingensmith G, Schatz D, et al. Diabetes care in the school and day care setting. Diabetes Care. 2013; 36 (Suppl 1): S75-9. [DOI:10.2337/dc13-S075]
13. Anderson BJ. Families and chronic illness research: Targeting transitions and tools--Commentary on Trief et al.(2006). Families, Systems and Health. 2006; 24(3): 332-5. [DOI:10.1037/1091-7527.24.3.332]
14. Saleh F, Mumu SJ, Ara F, Hafez MA, Ali L. Non-adherence to self-care practices & medication and health related quality of life among patients with type 2 diabetes: a cross-sectional study. BMC public health. 2014; 14 (1); 431. [DOI:10.1186/1471-2458-14-431]
15. Jermendy G, Erdesz D, Nagy L, Yin D, Phatak H, Karve S, et al. Outcomes of adding second hypoglycemic drug after metformin monotherapy failure among type 2 diabetes in Hungary. Health and Quality of Life Outcomes. 2008;6(1):1-8. [DOI:10.1186/1477-7525-6-88]
16. Prajapati VB, Blake R, Acharya LD, Seshadri S. Assessment of quality of life in type II diabetic patients using the modified diabetes quality of life (MDQoL)-17 questionnaire. Brazilian Journal of Pharmaceutical Sciences. 2017; 53(4): 1-9. [DOI:10.1590/s2175-97902017000417144]
17. Snoek FJ. Quality of life: A closer look at measuring patients' well-being. Diabetes Spectrum. 2000; 13(1): 24-8.
18. Acharya LD, Shaistakareem, Farooq KK A, Mallayasamy S. Development and validation of quality of life assessment instrument for diabetic patients. Asian Journal of Pharmaceutical and Health Sciences. 2014; 4(4): 1114-20.
19. Rubin RR, Peyrot M. Quality of life and diabetes. Diabetes/metabolism research and reviews. 1999; 15(3): 205-18. [DOI:10.1002/(SICI)1520-7560(199905/06)15:33.0.CO;2-O]
20. Kiadaliri A, Najafi B, Mirmalek-Sani M. Quality of life in people with diabetes: A systematic review of studies in Iran. Journal of Diabetes & Metabolic Disorders. 2013; 12(1): 1-10. [DOI:10.1186/2251-6581-12-54]
21. Toobert DJ, Hampson SE, Glasgow RE. The summary of Diabetes self-care activities measure: Results from 7 studies and a revised scale. Diabetes Care. 2000; 23(7): 943-50. [DOI:10.2337/diacare.23.7.943]
22. Pourisharif H, Babapour J, Zamani R, Besharat MA, Mehryar AH, Rajab A. The effectiveness of motivational interviewing in improving health outcomes in adults with type 2 Diabetes. Procedia-Social and Behavioral Sciences. 2010; 5: 1580-4. [DOI:10.1016/j.sbspro.2010.07.328]
23. Ware Jr JE, Kosinski M, Keller SD. A 12-item short-form health survey: Construction of scales and preliminary tests of reliability and validity. Medical Care. 1996: 32(3): 220-33. [DOI:10.1097/00005650-199603000-00003]
24. Montazeri A, Vahdaninia M, Mousavi SJ, Omidvari S. The Iranian version of 12-item short form health survey (SF-12): Factor structure, internal consistency and construct validity. BMC Public Health. 2009; 9(1): 341-0. [DOI:10.1186/1471-2458-9-341]
25. Ausili D, Bulgheroni M, Ballatore P, Specchia C, Ajdini A, Bezze S, et al. Self-care, quality of life and clinical outcomes of type 2 Diabetes patients: An observational cross-sectional study. Acta Diabetologica. 2017; 54(11): 1001-8. [DOI:10.1007/s00592-017-1035-5]
26. Koponen AM, Simonsen N, Suominen S. Determinants of physical activity among patients with type 2 Diabetes: The role of perceived autonomy support, autonomous motivation and self-care competence. Psychology, Health & Medicine. 2017; 22(3): 332-44. [DOI:10.1080/13548506.2016.1154179]
27. Egan A, Mahmood W, Fenton R, Redziniak N, Kyaw Tun T, Sreenan S, et al. Barriers to exercise in obese patients with type 2 Diabetes. QJM: An International Journal of Medicine. 2013; 106(7): 635-8. [DOI:10.1093/qjmed/hct075]
28. Delahanty LM, Grant RW, Wittenberg E, Bosch JL, Wexler DJ, Cagliero E, et al. Association of diabetes-related emotional distress with diabetes treatment in primary care patients with Type 2 Diabetes. Diabetic Medicine : A Journal of the British Diabetic Association. 2007; 24(1): 48-54. [DOI:10.1111/j.1464-5491.2007.02028.x]
29. Gonzalez JS, Esbitt SA, Schneider HE, Osborne PJ, Kupperman EG. Psychological issues in adults with type 2 Diabetes. In: Pagoto S, editor. psychological co-morbidities of physical illness: A behavioral medicine perspective. New York, NY: Springer New York; 2011: 73-121. [DOI:10.1007/978-1-4419-0029-6_2]
30. Poorgharahkhan A, Hekmatpou D, Javaherie A, Takhti A. The effect of factors satisfaction of disease control and self-care behavior on quality of life of patients with Diabetes mellitus type 2. Journal of Clinical Nursing and Midwifery. 2016;5(2). 64-74. [In Persian].
31. Amelia R. The model of self care behaviour and the relationship with quality of life, metabolic control and lipid control of type 2 Diabetes mellitus patients in Binjai city, Indonesia. Open Access Macedonian Journal of Medical Sciences. 2018; 6(9): 1762-7. [DOI:10.3889/oamjms.2018.363]
32. İlhan N, Telli S, Temel B, Aştı T. Health literacy and diabetes self-care in individuals with type 2 Diabetes in Turkey. Primary Care Diabetes. 2021; 15(1): 74-9. [DOI:10.1016/j.pcd.2020.06.009]
33. Jannoo Z, Wah YB, Lazim AM, Hassali MA. Examining diabetes distress, medication adherence, diabetes self-care activities, diabetes-specific quality of life and health-related quality of life among type 2 Diabetes mellitus patients. Journal of Clinical & Translational Endocrinology. 2017; 9: 48-54. [DOI:10.1016/j.jcte.2017.07.003]
34. Baraz S, Zarea K, Shahbazian HB. Impact of the self-care education program on quality of life in patients with type II diabetes. Diabetes & Metabolic Syndrome: Clinical Research & Reviews. 2017; 11(2): S1065-S8. [DOI:10.1016/j.dsx.2017.07.043]
35. O'Shea MP, Teeling M, Bennett K. Comorbidity, health-related quality of life and self-care in type 2 Diabetes: A cross-sectional study in an outpatient population. Irish Journal of Medical Science (1971-). 2015; 184(3): 623-30. [DOI:10.1007/s11845-014-1190-4]
36. Rintala T-M, Jaatinen P, Paavilainen E, Åstedt-Kurki P. Interrelation between adult persons with diabetes and their family: a systematic review of the literature. Journal of family nursing. 2013;19(1): 3-28. [DOI:10.1177/1074840712471899]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |